EMR Integration Success Story: A Small Clinic’s Actual Experience
💡 A small clinic fixed its biggest workflow bottlenecks by integrating communication with its EMR. Before: Staff spent hours on phones, patients...
8 min read
Gregory Vic Dela Cruz : Updated on August 26, 2025
For any medical practice, healthcare workflow bottlenecks show up as daily friction. Tasks take longer than they should, calls stack up, and staff spend more time moving information than caring for people. But these slowdowns are avoidable when tools "talk" to each other. That's where the value of proper integration comes in, However, when your tools fail to connect—when your EMR, scheduling, intake, and messaging are siloed—operational issues compound into lost time, revenue, and patient trust. In short, common EMR workflow issues become problems with the patient experience.
In this article, we will:
If your front desk feels overwhelmed or your schedule swings from overbooked to underutilized, this guide will help you pinpoint the bottlenecks. Let's learn how to fix them with integration, automation, and secure two-way patient communication.
Patient experience isn’t a soft metric; it’s the full range of interactions patients have with your practice—from first contact to post-visit follow-up. The Agency for Healthcare Research and Quality (AHRQ) defines it as the patient’s interactions across settings and staff, making it a core pillar of care quality. When your electronic systems are disconnected, those interactions become fragmented: calls bounce between departments, instructions contradict, and simple tasks take too long. The experience degrades before the patient even arrives.
Disconnection shows up as operational friction: appointment data lives in one place; reminders are handled in another; forms are on paper; and messaging happens ad hoc. Staff are forced to re-enter data, track down updates, and chase patients by phone. This wastes time and introduces avoidable errors—missed notes, outdated instructions, or duplicate entries that confuse both staff and patients. The result? Longer response times, less transparency, and lower trust.
For patients, the cost is convenience and confidence. They expect seamless digital communication—confirmation texts, easy rescheduling, and pre-visit forms they can fill out from their phone. When those essentials break, patients experience uncertainty (“Did my forms go through?”), anxiety (“Where do I go?”), and frustration (“I already told you my insurance info”). Over time, these small failures accumulate into dissatisfaction and churn—especially when competing clinics offer a smoother journey.
From a revenue standpoint, fragmentation creates no-shows and same-day cancellations. Without integrated reminders and two-way messaging, many patients fail to confirm or can’t easily reschedule. Clinics that connect reminders to their EMR—and allow quick confirmations, cancellations, and rebooking—routinely see no-show rates fall dramatically. Conversely, practices that rely on manual calls or disconnected systems lose billable visits and scramble to backfill schedules.
Interoperability is not just a technical preference; it’s a patient-experience requirement. National policy has moved firmly toward patient access and interoperability, including information blocking rules and API requirements that make it easier for patients to access and manage their information with apps of their choice. This push recognizes that timely, coordinated access to information improves the care experience and supports better outcomes.
Staff experience matters too. When systems don’t speak, your team bears the burden: searching for records, juggling spreadsheets, and returning calls. That administrative drag is a leading driver of burnout—time that could have gone into empathetic, proactive patient service instead gets consumed by “system work.” Integrating communication with the EMR reverses that dynamic, letting staff focus on patients while software handles the repetitive tasks.
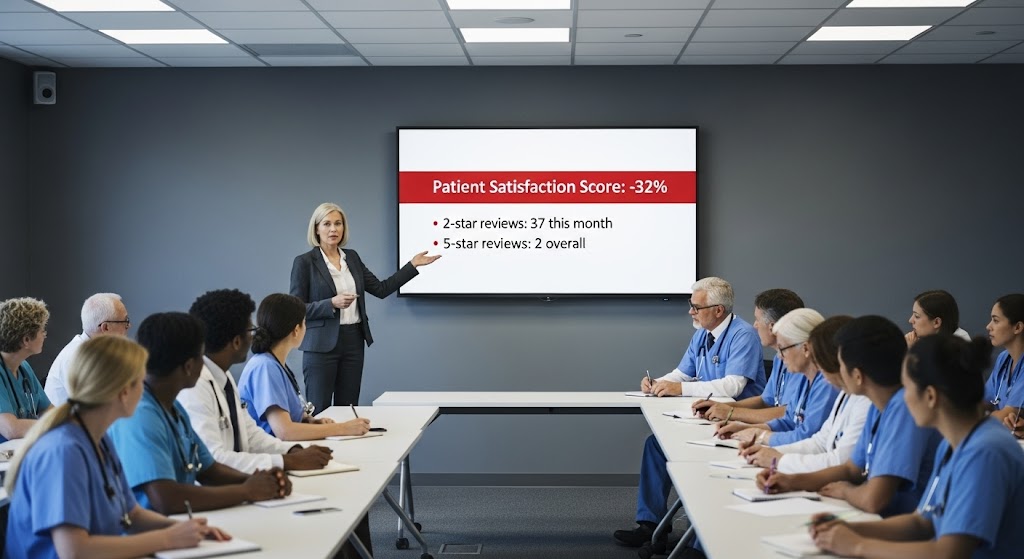
Disconnected systems also weaken feedback loops. Without integrated surveys and review prompts, you miss timely patient input that could fix a process. Tying automated post-visit surveys to visit types and outcomes helps you capture experience data, act on it quickly, and amplify positive reviews—strengthening both patient satisfaction and online reputation.
In short, if your EMR, scheduling, forms, and messaging are siloed, patients feel the lag as longer waits, confusing instructions, and limited self-service. Integrated workflows—especially HIPAA-compliant 2-way texting, automated reminders, and online intake—replace friction with clarity. They make patient interactions faster, simpler, and more respectful of people’s time.
What breaks: Patients call to book, land on hold, and later receive disconnected reminders (or none at all). Pre-visit instructions arrive late or contradict the portal. New patients are handed clipboards onsite, creating long check-in lines and transcription errors. Each friction point raises anxiety and increases no-show risk.
Integration fix: Connect the EMR schedule to automated, customizable appointment reminders and two-way texting so patients can confirm, cancel, or reschedule instantly. Trigger digital intake packets tied to appointment type (e.g., MRI prep vs. annual wellness), reducing confusion and preparing patients properly. Practices using integrated reminders and online forms consistently cut phone volume and lower no-shows—boosting capacity and staff focus.
What breaks: Paper forms, manual insurance capture, and re-keying data create delays. Patients feel like they repeat themselves across staff and systems. Missed updates (e.g., allergies, meds) become safety and experience risks.
Integration fix: Pre-visit intake data should flow into the EMR to validate demographics, insurance, consents, and clinical history before the visit. A HIPAA-compliant communication layer can nudge late patients, route them to the correct location, and surface prep instructions on demand. The payoff is a shorter, calmer check-in—an early trust signal that sets the tone for the visit.
What breaks: Clinicians lack outside records or must dig through multiple systems, leading to repeat questions and missed context. That erodes confidence: patients wonder why their care team doesn’t “know them.”
Integration fix: Interoperability improves the availability and use of patient information at the point of care. Hospitals that routinely engage in interoperable exchange see significantly higher clinician use of external information for decision-making—supporting safer, more coordinated care that patients can feel.
What breaks: Patients leave with paper instructions they might misplace. Follow-up reminders are inconsistent. Questions pile up on the phone queue, and staff struggle to triage messages quickly.
Integration fix: Tie post-visit instructions, labs, and follow-up tasks to automated, secure messages—so patients can ask questions, receive guidance, and complete next steps without waiting on hold. Integrated post-visit surveys capture timely feedback, enabling service recovery and generating positive reviews to strengthen reputation.
Interoperability and patient-facing APIs—including smartphone access—expand access for more patients (and caregivers) by making health information portable and timely. Federal policy continues to push for this capabilities growth, and providers that lean in will meet patient expectations for convenience and transparency—key drivers of satisfaction and loyalty.
Patient experience is broader than satisfaction scores; it’s the lived flow of information and service. Value-based models are elevating outcomes and experience measures together—meaning your integration strategy directly influences quality metrics and reimbursement. When the EMR, scheduling, forms, and messaging are integrated, patients move through each stage with confidence. They know where to go, what to do, and how to reach you. Staff spend less time on manual calls and more time on empathetic service. That is experience design—powered by interoperability.

Great experiences aren’t accidents—they’re orchestrated by an integrated architecture that puts patients (and staff) at the center. Here’s the blueprint clinics use to turn disconnected tools into one coordinated system.
Replace “phone-tag” with a shared inbox for 2-way texting, routed by location/provider. Templates standardize responses; saved replies accelerate common tasks (refills, forms, directions). This model routinely reduces phone volume by 50%, freeing staff to handle high-value work and complex cases.
Integrated, customizable reminders are the linchpin. Send at patient-friendly intervals (e.g., 7 days, 72 hours, 24 hours, 2 hours) with clear actions: confirm, cancel, or reschedule. Tie content to appointment type (e.g., fasting, meds hold, paperwork). Practices commonly reduce no-shows by up to 75% with this approach. Service pages and case guides echo these gains across specialties.
Digitize registration, histories, consents, and insurance uploads. Patients complete forms from any device before arrival; staff validate and import directly into the EMR to remove duplicate entry and errors. Result: shorter lines, fewer frustrations, cleaner data.
For virtual visits, send secure links and tech checks via automated messages so patients join on time. After the visit, deliver instructions, labs, and educational materials through secure channels, then trigger a post-visit survey. This closes the loop and supports continuous improvement. Providers adopting HIPAA-compliant texting for telehealth report better engagement and faster scheduling—benefits patients feel.
7. What to Measure (Experience KPIs)
Patient-focused EMR integration means connecting schedule, intake, messaging, telehealth, and survey loops so the journey feels intuitive. The outcomes—fewer calls, fewer no-shows, faster visits—are the operational expression of respect for patients’ time.
When patients encounter delays, duplicate questions, or unclear instructions, they lose confidence in you as a healthcare provider. In today’s competitive healthcare landscape, experience is as critical as clinical quality. Disconnected systems chip away at that experience, leaving patients frustrated and staff burned out.
The solution is clear: patient experience EMR integration. By connecting scheduling, reminders, intake, communication, and feedback in one secure platform, practices can cut no-shows, reduce calls, and deliver a care experience patients actually value.
Curogram makes this transformation achievable—without ripping and replacing your EMR. It’s affordable, HIPAA-compliant, and designed around the real workflows of front-desk staff and providers. The result is a practice that runs more efficiently, with patients who are more satisfied and loyal.
Interested? Book your free demo today and see how Curogram can eliminate workflow bottlenecks and elevate your patient experience.

💡 A small clinic fixed its biggest workflow bottlenecks by integrating communication with its EMR. Before: Staff spent hours on phones, patients...
.png)
💡Clinic workflow management is the system that keeps a medical practice running smoothly. It covers every step—from patient intake to scheduling,...
-1.png)
💡Missed appointments are one of the biggest hidden costs in healthcare. On average, 20–30% of patients skip scheduled visits. This has led to...