Before vs. After Integration: EMR Integration Daily Workflow Changes
💡Clinic workflow integration changes everything. Before integration, staff juggle phone calls, paperwork, and disconnected systems. After...
7 min read
Gregory Vic Dela Cruz : August 30, 2025
.png)
If there's one thing healthcare leaders can agree on, it's that the patient care experience can be better. More and more, practitioners and administrators are seeing the value of integration. But the challenge isn’t deciding whether your practice should integrate. Rather, it’s knowing where to begin.
Should you start with appointment scheduling? Digital intake? Patient communication? Billing and collections? Each area has compelling reasons, but not all yield the same immediate return on investment.
Think of it like renovating a house. You wouldn’t tear down every wall at once; you’d prioritize the space that creates the most value quickly while setting a foundation for future improvements. The same principle applies to healthcare workflow integration. The first step should address a visible pain point that staff and patients feel every day. At the same time, you should also stay focused on strategic goals like lowering no-shows, improving collections, or cutting phone call volume.
This blog will help you identify the right “first integration” for your practice. We’ll explore the most common bottlenecks—scheduling, intake, communication, and billing—and help you assess where integration will pay off fastest. Keep reading to learn more on the exact next steps your practice should take.
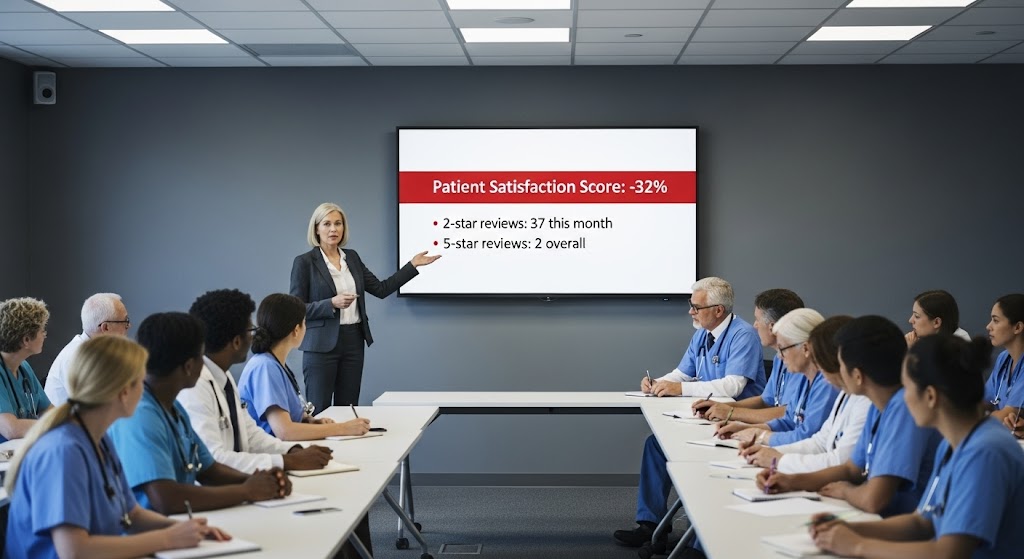
Every healthcare practice experiences the drag of disconnected workflows. Staff waste time moving data between systems, patients get frustrated with inconsistent communication, and administrators lose revenue due to inefficiency. These aren’t small inconveniences—they are systemic problems that compound daily. Below, we examine the five most pressing risks of delaying workflow integration and how they undermine patient care and clinic performance.
Scheduling is the heartbeat of any clinic. Yet in many practices, the EMR houses the schedule while patient reminders come from a separate tool, or worse, from staff phone calls. Without integration, reminders are inconsistent, often inaccurate, and rarely trackable. Patients may confirm by phone but fail to appear in the EMR as “confirmed,” leaving staff uncertain and providers with unexpected gaps.
This chaos affects everyone. Providers lose revenue when no-shows climb above industry averages of 15–30 percent. Patients wait longer for appointments because open slots go unfilled. Administrators face the impossible task of predicting daily revenue when schedules collapse at the last minute. Without integration, scheduling remains one of the costliest inefficiencies in healthcare operations.
Check-in often feels like stepping back in time. Clipboards, pens, and stacks of forms remain standard in too many clinics. But paper intake isn’t just outdated—it’s harmful. Staff re-enter demographics, insurance details, and medical histories into the EMR, multiplying opportunities for error. A single digit off in an insurance ID can result in a denied claim, while an incomplete allergy history could compromise patient safety.
The problem doesn’t stop at data entry. Paper forms create bottlenecks in the waiting room, frustrate patients, and slow down providers who start visits with incomplete or illegible information. These inefficiencies cascade downstream into billing, compliance, and care quality.
Patient communication is often the first point of contact and the primary source of frustration. Without integration, communication is fragmented across voicemails, sticky notes, and unmonitored inboxes. Patients may call to reschedule, only for that message to get lost before reaching the right staff member. Others receive reminders that don’t match their actual appointment times, leading to missed visits and angry patients.
Staff, meanwhile, spend hours fielding repetitive calls about directions, prep instructions, and insurance policies. Without integration, these conversations must be logged manually—if they are logged at all—creating compliance gaps and increasing the chance of errors. Inefficient communication drives patient dissatisfaction and overwhelms staff with busywork.
Revenue cycle inefficiency is one of the most painful consequences of disconnected workflows. When intake data does not flow directly into billing systems, claims are submitted with errors or missing information. This leads to denials, rework, and long delays in reimbursement. Patients, too, face frustration with mailed statements that arrive weeks after visits or unclear balances that require phone calls to resolve.
The result is slow collections and significant revenue leakage. Accounts receivable grows as balances linger for 30, 60, or 90 days. Staff spend hours making collection calls that patients ignore. Administrators lose visibility into financial performance, unable to predict or control cash flow. For many practices, disconnected billing workflows are the difference between stable revenue and chronic financial stress.
At the core of all these issues are the staff tasked with managing them. Front-desk employees juggle phones, data entry, and patient complaints while toggling between multiple systems. Billing staff chase claims and collections manually. Nurses document information twice—once in the EMR and again in the patient portal. This repetitive, reactive work erodes morale quickly.
Burnout isn’t just a human cost—it’s a business one. High turnover increases recruiting and training expenses, disrupts operations, and diminishes patient experience. A burned-out staff can’t deliver compassionate care, and administrators pay the price in both dollars and reputation.
Fragmented systems create compliance blind spots that leave practices vulnerable. Staff texting patients from personal phones or sending instructions by unsecured email are common workarounds when official systems are too clunky or disconnected. Each of these shortcuts represents a potential HIPAA violation. Without unified, compliant communication, administrators gamble with patient trust and regulatory fines every day.
The risks of delaying workflow integration are clear: lost revenue, patient frustration, staff burnout, and compliance exposure. Each day without integration compounds inefficiency and erodes trust. To break this cycle, clinics must act strategically, starting integration where it will create the most immediate and visible impact.
.png?width=1024&height=535&name=healthcare-workflow-automation-workflow-integration-mid%20(1).png)
Knowing that integration is critical is one thing; deciding where to begin is another. For administrators, the first integration should deliver fast ROI, reduce visible pain points, and set the stage for broader transformation. Below, we examine four core workflows—scheduling, intake, communication, and billing—and provide practical guidance on when each should be your starting point.
Integrated scheduling links the EMR directly with communication tools, enabling automated, automated, two-way reminders. Patients can confirm, cancel, or reschedule by text, while updates flow instantly into the EMR. Clinics that implement integrated reminders typically see no-shows drop by 50–75 percent. This stabilizes provider utilization, improves patient access, and delivers a fast financial return.
Digital intake sends patients forms automatically before visits, allowing them to complete demographics, medical histories, and consents from their devices. Data flows directly into the EMR, eliminating duplicate entry. The benefits are measurable: check-in times drop by 50 percent or more, billing accuracy improves, and providers enter visits with complete, legible information. Patients perceive the process as modern and efficient, strengthening satisfaction scores.
Integrated communication creates a HIPAA-compliant shared inbox tied to the EMR. Staff can respond with context at their fingertips, using templates for common questions like directions, prep instructions, or insurance policies. Call volume decreases by 40–50 percent, patients get faster responses, and satisfaction scores climb. For staff, the shift from phones to texting reduces daily stress and boosts productivity.
Integrated billing enables text-to-pay features, pre-visit estimate requests, and automated balance reminders tied directly to the EMR. Patients pay balances quickly from their phones, eliminating the friction of mailed statements. Clinics that adopt text-to-pay report 30–40 percent faster collection cycles, stronger cash flow, and fewer staff hours spent on collections. This workflow is often the fastest path to financial stability.
The right first integration depends on your clinic’s most urgent problems and strategic goals:
Whichever workflow you choose, the first integration should create a quick, visible win. Success builds confidence among staff and leadership, making it easier to expand integration into other workflows. For example, a practice that reduces no-shows with automated reminders can then roll out digital intake to improve data accuracy. Each success compounds, creating momentum toward full integration.
Choosing which part of your workflow to integrate first is less about technology and more about strategy. Start where the pain is sharpest and the ROI is clearest. With each win, you’ll build trust, efficiency, and capacity for further integration—step by step transforming your practice from fragmented to seamless.
Curogram is designed to meet clinics where they are. Instead of forcing a full overhaul, it allows you to start integration in the workflow that needs it most and expand over time. Whether your first priority is reducing no-shows, eliminating paperwork, cutting call volume, or improving collections, Curogram delivers immediate results.
Clinics using Curogram report up to 75 percent fewer no-shows, 50 percent reductions in call volume, faster billing collections, and stronger patient satisfaction. Staff adoption is fast, with training typically taking less than 10 minutes. The platform integrates with nearly any EMR, ensuring flexibility across different practice environments.
By starting with the workflow that hurts most, Curogram ensures integration isn’t overwhelming—it’s practical, measurable, and scalable.
Every clinic wants the benefits of integration, but the question is where to begin. The answer lies in your pain points. If no-shows are draining revenue, start with scheduling. If paperwork and billing errors are overwhelming staff, start with digital intake. If communication is breaking down, start with messaging. If collections are slipping, start with billing integration.
Curogram makes it easy to start small and expand, delivering measurable wins quickly. With HIPAA-compliant reminders, digital intake, patient texting, and billing tools that sync directly to the EMR, clinics can eliminate their biggest inefficiencies in a matter of weeks.
Book your free demo with Curogram and see how workflow integration can transform your clinic step by step.

💡Clinic workflow integration changes everything. Before integration, staff juggle phone calls, paperwork, and disconnected systems. After...

💡 A small clinic fixed its biggest workflow bottlenecks by integrating communication with its EMR. Before: Staff spent hours on phones, patients...
💡EMR integration improves patient experience by eliminating data silos and delays across scheduling, intake, visits, and follow-up. With a...