Healthcare Workflow Automation 101: Reducing Bottlenecks and Friction
💡What are workflow bottlenecks in clinics?In disconnected systems, small handoff failures pile up and become huge delays. Manual re-entry, phone...
7 min read
Gregory Vic Dela Cruz : Updated on August 21, 2025
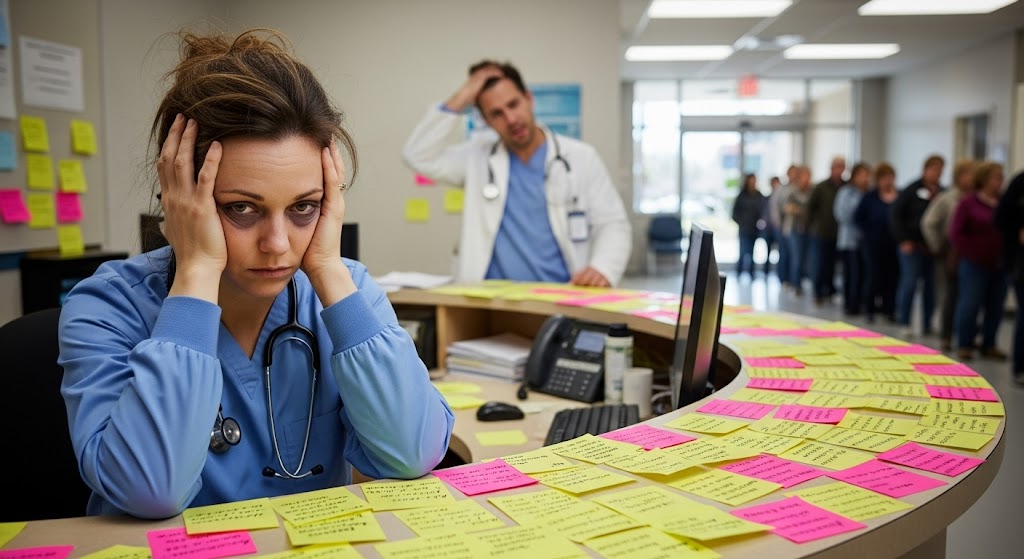
Administrative burnout in healthcare can easily be mistaken as a staffing issue. More often than not, however, it’s a systems issue. When front desk staff spend their day re-entering patient details, making endless reminder calls, and chasing down forms, it creates frustration and fatigue. These struggles are real examples of what truly causes admin burnout and why practices everywhere are searching for solutions that actually work.
In this blog, we’ll explore how workflow inefficiency from disconnected tools is the leading cause of admin burnout in clinics. This article will aim to:
You’ll also see real-world outcomes from practices that streamlined their communications and thus were able to reclaim time for meaningful work. By the end, you’ll know exactly how to reduce admin burnout in your practice while boosting patient satisfaction and revenue.
Admin burnout in healthcare describes the exhaustion and disengagement staff feel when their workload is dominated by repetitive, manual tasks. Unlike clinical burnout, which gets more attention, admin burnout often goes unnoticed until it affects patient care and revenue. When staff morale drops, turnover increases, and productivity declines, the entire organization feels the strain. Research suggests that inefficient workflows are one of the top contributors to healthcare staff burnout, creating a cycle of stress and disengagement that is hard to reverse without system changes.
Over time, these issues chip away at job satisfaction. Talented staff members leave for less stressful roles, turnover costs rise, and clinics lose valuable experience. This is why tackling workflow inefficiency is central to solving admin burnout healthcare challenges.
Administrative burnout in healthcare is often underestimated because its effects don’t show up as a line item in financial statements. Yet the costs are very real—lost productivity, higher turnover, increased compliance risks, and a decline in patient satisfaction. To understand the full picture, it helps to look at how burnout plays out in three core areas: revenue, compliance, and patient care.
One of the biggest impacts of administrative burnout is on a clinic’s bottom line. When staff spend large portions of the day on repetitive, manual tasks such as re-entering data or making phone calls, they have less time to support revenue-generating activities. Missed opportunities can include scheduling additional patients, following up on outstanding balances, or coordinating preventive care visits. Studies estimate that each missed appointment costs a practice between $150 and $300, and high no-show rates can drain tens of thousands of dollars annually.
Burned-out staff are also more likely to make mistakes that require costly fixes—incorrect billing codes, misplaced insurance information, or incomplete forms that delay claims. These errors slow down reimbursement cycles and contribute to cash flow challenges. In the long term, high staff turnover compounds the issue. Replacing and training new employees not only costs money but also disrupts productivity during the transition period. Ultimately, unchecked burnout turns into recurring revenue leakage that can erode profitability.
Burnout doesn’t just affect efficiency—it can create serious compliance vulnerabilities. Healthcare administrators are responsible for handling sensitive patient data, ensuring that communication is HIPAA-compliant, and maintaining accurate documentation. When staff are exhausted and juggling multiple disconnected systems, the risk of errors increases significantly.
Examples include sending patient reminders through unsecured channels, forgetting to document verbal communications, or mishandling consent forms. Each of these mistakes may expose the clinic to HIPAA violations, which can result in fines ranging from $100 to $50,000 per violation. Beyond financial penalties, compliance breaches damage a clinic’s reputation and erode patient trust. Patients expect their information to be protected, and even a single incident can create long-term reputational harm.
Burnout also contributes to gaps in audit trails. If communication is scattered across phone calls, sticky notes, and personal email accounts, it becomes nearly impossible to provide the documentation required in an audit. This lack of standardized processes not only increases legal exposure but also puts accreditation and payer contracts at risk. In short, burnout doesn’t just cause stress for staff—it creates tangible compliance liabilities for the entire practice.
Perhaps the most concerning impact of administrative burnout is the effect it has on patient care. Burned-out staff are less likely to be responsive, empathetic, and thorough in their communication. This can lead to slower response times, missed messages, or incomplete follow-ups—all of which frustrate patients and reduce their trust in the practice.
For example, when staff are overwhelmed by call volume, patients may struggle to get quick answers to simple questions. Delays in confirming appointments or providing procedure prep instructions lead to confusion and increase the likelihood of cancellations or no-shows. Patients who feel neglected are less likely to return and more likely to leave negative online reviews, which directly affects the clinic’s reputation and ability to attract new patients.
Over time, a cycle develops: burned-out staff provide less satisfactory service, which frustrates patients, leading to more calls, more complaints, and more stress for the staff. Without intervention, both staff morale and patient experience spiral downward. For practices operating in competitive healthcare markets, this can be devastating—patients will often choose another provider who offers better communication and a smoother experience.
Revenue loss, compliance risk, and patient dissatisfaction don’t happen in isolation—they compound one another. A single compliance issue can reduce patient trust and lower satisfaction. High staff turnover disrupts workflows, which further increases errors and lowers productivity. Dissatisfied patients lead to fewer appointments, less revenue, and more pressure on the staff who remain. This interconnected web of problems is why administrative burnout is not just an HR issue but a business-critical challenge.
Ultimately, the cost of ignoring burnout is far greater than the investment required to fix it. By addressing workflow inefficiency and giving staff modern tools that integrate with EMRs, clinics can break this cycle. The result is not only healthier, more engaged employees but also stronger financial performance, improved compliance, and happier patients.

The fastest way to reduce admin burnout in healthcare is to eliminate repetitive tasks and communication bottlenecks. While staff training and wellness initiatives help, they don’t solve the root cause—inefficient systems. The true solution lies in integration. By connecting EMRs with communication tools, practices transform how daily tasks are handled. Instead of juggling disconnected platforms, everything flows through a single, HIPAA-compliant hub.
Let’s explore how EMR integration combined with Curogram’s automation tools helps practices cut through inefficiency and restore balance for staff.
Most clinics struggle because their EMRs weren’t designed for patient-friendly communication. Staff end up retyping appointment details, manually confirming visits, or printing intake forms for scanning—all of which drains time and morale. Curogram solves this by integrating directly with nearly any EMR, creating a seamless connection between the patient record and communication tools.
Appointment data flows automatically, so reminders and confirmations are triggered without staff intervention. Intake forms submitted online sync directly to the chart, eliminating double entry and reducing errors. This integration means that what patients submit, confirm, or request outside the clinic is visible inside the EMR in real time.
The result? Staff stop acting as “human bridges” between systems. They no longer need to copy and paste details or manage multiple software tabs to keep patient records updated. By cutting out these low-value tasks, EMR integration directly reduces burnout and frees up staff to focus on meaningful patient interactions.
No-shows are a major stressor for administrative teams, who spend hours making calls to confirm or reschedule. With Curogram’s EMR-connected reminders, this process becomes automatic. The system sends texts or emails that pull directly from the EMR, ensuring accuracy and timeliness.
Patients can confirm or reschedule with a simple reply, and the EMR updates automatically. This eliminates the back-and-forth calls that weigh staff down and fills the schedule more efficiently. Clinics using this feature report up to a 75% reduction in no-shows, directly improving revenue while reducing staff workload.
Phone calls are one of the biggest contributors to healthcare workflow inefficiency. Staff spend countless hours answering routine questions, confirming visits, or leaving voicemails that patients may never check. Curogram replaces these phone calls with secure two-way texting.
Because the system integrates with the EMR, every message is logged, and staff can see the context of the appointment while chatting. Patients can ask questions, send photos, or update their status—all through their mobile device. For staff, this means fewer interruptions and faster resolutions. For patients, it means communication on their terms, leading to higher satisfaction and fewer missed details.
Paper intake forms are another burnout driver. Staff must print, scan, and type information into the EMR, often under time pressure at check-in. Curogram replaces this with online, HIPAA-compliant forms that patients complete before their visit.
Once submitted, the forms sync automatically with the EMR. Staff no longer need to re-enter information, and providers have complete patient data available at the start of the appointment. This reduces administrative workload, speeds up check-in, and decreases the likelihood of errors—making workflows smoother for both staff and patients.
Billing follow-up calls are another drain on staff energy. Curogram’s text-to-pay feature automates balance reminders and allows patients to pay securely from their phones. Because payments are logged into the EMR and billing system, staff don’t have to chase balances or manually update records. This not only accelerates collections but also reduces the awkwardness of financial conversations during check-in, a major stress point for administrative teams.
What sets Curogram apart is how all of these features connect through EMR integration. Each tool—reminders, two-way texting, online forms, text-to-pay—relieves a specific pain point. But the real value comes when they work together seamlessly inside the EMR. Staff gain one connected workflow instead of multiple disconnected tasks. This shift reduces administrative burden, minimizes errors, and gives teams confidence that patient data is accurate and up to date. Ultimately, EMR integration is not just a technology upgrade; it’s a direct intervention against administrative burnout.
With integration in place, staff can breathe again. Instead of working as system operators, they can return to their true role—supporting patients. That change not only improves employee morale but also enhances patient experience and drives better business outcomes for the clinic.
Practices that fix healthcare workflow inefficiency report measurable results almost immediately:
Administrative burnout isn’t inevitable. Workflow inefficiency can be fixed with the right systems. By integrating your EMR with modern communication tools, your practice can reduce staff burden, cut waste, and give your patients the seamless experience they expect. Everyone wins: staff reclaim time, patients feel supported, and the practice grows stronger.
Book your free demo with Curogram today and see how you can help your team members perform their best while valuing their well-being.

💡What are workflow bottlenecks in clinics?In disconnected systems, small handoff failures pile up and become huge delays. Manual re-entry, phone...
.png)
💡The key to improve clinic efficiency lies in strategies that reduce admin burden. Doing so improves patient flow without hiring and increases...

💡Clinic workflow integration changes everything. Before integration, staff juggle phone calls, paperwork, and disconnected systems. After...