Behavioral Health Clinical Texting: Convert More Leads Fast
💡 Behavioral health clinical texting helps addiction treatment centers convert more leads into admissions by enabling instant, secure communication...
12 min read
.jpg) Mira Gwehn Revilla
:
Updated on February 17, 2026
Mira Gwehn Revilla
:
Updated on February 17, 2026

In addiction treatment, time is more than money. It can mean the difference between a patient starting their recovery or walking out the door.
Every minute a person waits in your lobby is a minute they might change their mind. Paper forms, slow data entry, and long waits create friction. That friction costs your facility real dollars and real lives.
There is a better way, however. Digital patient intake for Opus EHR removes the roadblocks that slow down admissions. It moves the process from your front desk to the patient's phone. This change can transform how your facility operates.
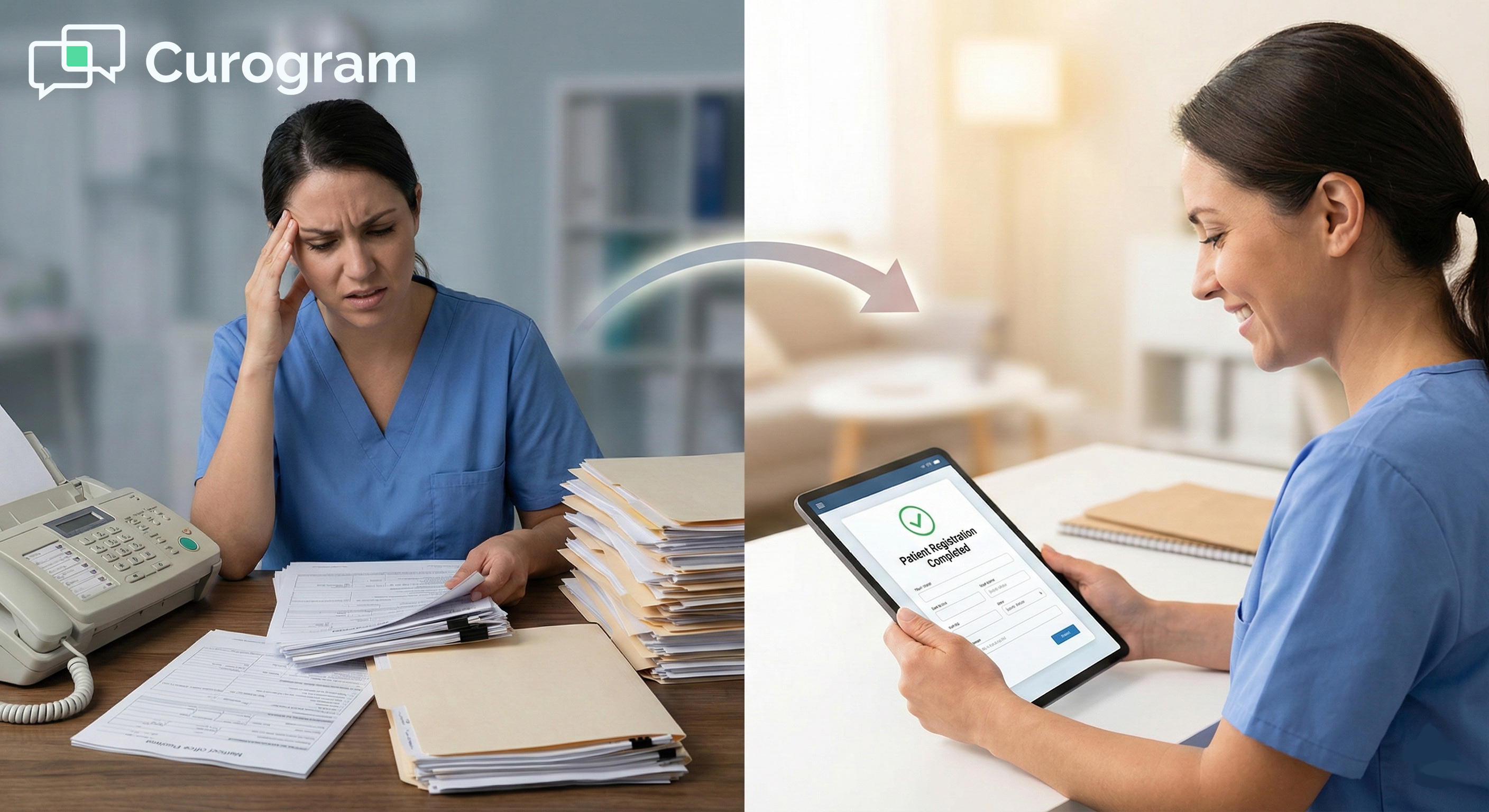
Think about what happens today when a new patient arrives. Your staff hands them a clipboard. They fill out page after page of forms. Then someone types all that data into your EHR. This takes time. It costs money. And it puts your admission at risk.
Now, picture a different approach. The patient gets a text with a link to fill out forms on their phone. They do this at home, in the car, or wherever they feel ready. When they arrive, their data is already in Opus. Your team greets them, not with paper, but with care.
This is not just about saving time. It is about saving admissions. It is about boosting your addiction treatment admissions ROI in a way you can measure and prove.
In this article, we will break down the hidden costs of paper-based intake. We will show you how digital tools can reduce rehab intake time and boost behavioral health operational efficiency. Most importantly, we will give you real numbers to share with your CFO.
Let us start by looking at what paper-based intake really costs your facility.
Paper forms seem cheap. You buy a stack of forms, hand them to patients, and move on. But the true cost of paper-based intake goes far beyond the price of paper. It hides in your labor hours, your lost admissions, and your storage closets.
Let us break down these hidden costs one by one:
Your front desk staff spends a lot of time on data entry. Think about what happens after a patient fills out paper forms. Someone on your team has to type every answer into Opus EHR by hand.
Here is a simple example:
If your staff member earns $25 per hour and spends 45 minutes entering one patient's data, that task costs you nearly $20. Now, multiply that by 20 admissions per week. That is $400 per week just on data entry. Over a year, you are looking at more than $20,000 in labor costs for one task alone.
This does not include the time spent fixing errors. Handwriting can be hard to read. Names get misspelled. Dates get entered wrong. Each mistake takes more time to correct. This labor tax is a real drain on your budget.
Long waits in the lobby are not just annoying. They are risky. A person seeking treatment for substance use is often in a fragile state. The longer they sit with a clipboard, the more time they have to second-guess their choice.
Many facilities see patients leave AMA before treatment even starts. AMA stands for Against Medical Advice. Each lost admission is a missed chance to help someone. It is also lost revenue for your facility.
Consider this scenario:
A patient drives an hour to your facility. They sit in the lobby for 45 minutes filling out forms. During that time, their anxiety builds. They start to doubt. A family member outside sends a text asking them to come home. They walk out.
That empty bed could have generated thousands of dollars in revenue. More importantly, that patient did not get the help they needed. Reducing wait time is one of the best ways to protect both your mission and your bottom line.
Paper forms require paper, toner, and printers. These costs add up over time. But the bigger expense is storage. HIPAA rules require you to keep patient records for years. For paper files, that means secure filing cabinets, locked rooms, and often off-site storage.
Many facilities spend hundreds of dollars per month just to store old paper files. They also spend staff time pulling files when needed for audits or patient requests.
Digital systems remove this burden. Files live in the cloud. They take up no physical space. They are easier to search and retrieve.
When you look at labor, lost admissions, and material costs together, the clipboard cost is huge. Most facilities do not track these expenses because they seem normal. Paper has always been part of healthcare. But normal does not mean cheap.
The admissions department cost savings from going digital can be striking. You cut labor hours. You reduce no-shows. You eliminate storage fees. The money you save can go toward what matters most, helping more patients get better care.
Digital intake also supports better Opus EHR ROI. When data flows directly into your system, your team can focus on clinical work instead of typing. This shift improves behavioral health operational efficiency across your whole facility.
In addiction treatment, there is a saying: speed to bed. The faster you move a patient from first contact to their first day of treatment, the more likely they are to stay. Digital intake is a key tool to make this happen.
Let us look at how it works in practice:
Insurance matters. Before you can admit a patient, you need to verify their benefits. This process is called Verification of Benefits, or VOB. It tells you what services are covered and how much the patient or family will owe.
In a paper-based system, VOB can take hours or even days. Staff have to call the patient back to get insurance details. They might ask the patient to fax or email a copy of their card. Then they wait for the insurance company to respond.
Digital intake changes this flow. You send the patient a link by text message. They snap a photo of their insurance card right from their phone. That image goes straight to your team.
They can start the VOB process while the patient is still at home. By the time the patient arrives, you know what is covered.
This speed matters. Families in crisis do not want to wait. If you can give them clear answers fast, they are more likely to choose your facility over one that makes them wait.
When patients invest time in completing digital forms, they build commitment. This is a simple idea from psychology. The more effort someone puts into a decision, the more likely they are to follow through.
Think about this:
A patient who has already filled out 10 pages of forms on their phone. They have shared personal details about their history. They have signed consents. They are mentally ready. This patient is far less likely to skip their intake than someone who has done nothing yet.
This effect protects your marketing ROI. You spend money to generate leads. You spend staff time on phone calls and outreach.
When a patient no-shows, all that effort goes to waste. Digital intake helps you lock in that commitment early. It turns a "maybe" into a "yes."
Patients hate repeating themselves. If they tell your call center their address, then write it on a form, then say it again to a nurse, they get frustrated. This kind of friction makes your facility feel disorganized. It does not match the high-end experience patients expect.
Digital forms solve this problem. When a patient enters their data once, it flows into Opus EHR. That data can then pre-fill other forms. The patient does not get asked the same question five times. Your staff does not have to type the same answer five times.
This approach creates a smoother, more professional intake. It mirrors what patients see at top-tier hospitals and clinics. When you streamline SUD onboarding this way, patients feel cared for from the start.
Here is how this might look at your facility:
A family calls on Monday morning. By Monday afternoon, they have completed all forms on their phones. Your team has verified insurance. The patient arrives on Tuesday and walks straight into their first session.
Compare that to a paper-based flow:
The same family calls Monday. They come in Tuesday but spend an hour in the lobby with forms. Staff spend another hour on data entry. The patient does not start treatment until Wednesday.
That one-day difference adds up. It means more beds filled. It means more patients who stay instead of leaving. It means better outcomes for your facility and the people you serve.

Digital intake does more than save time at the front door. It changes how your entire facility works. When data flows smoothly into Opus EHR, every team benefits.
Let us look at the three biggest areas of impact:
Your admissions team did not train to be data entry clerks. They trained to help people in crisis. They know how to talk to a scared parent at 2 a.m. They know how to calm a patient who is having second thoughts. These are high-value skills.
But in a paper-based system, much of their day goes to typing. They take information from a form and enter it into the computer. This task requires no special training. Anyone can do it. Yet your skilled admissions staff spend hours on it every week.
Digital intake lets your team focus on what they do best. When forms come in already filled out, staff can review data instead of entering it. They can spend more time on clinical screening. They can call families back faster. They can handle more leads.
Here is a concrete example:
Say your admissions coordinator can handle 5 new patient calls per day in a paper-based system. Much of their time goes to paperwork after each call. With digital intake, that same person might handle 8 or 10 calls per day. They become more effective without working longer hours.
This shift has real value. You do not need to hire more staff to grow your census. You just need to free up the staff you already have. This is one of the clearest ways digital intake drives behavioral health operational efficiency.
Billing mistakes cost money. When a claim gets rejected, your team has to fix it and resubmit. This takes time. It also delays your cash flow. The gap between service and payment can stretch from days to weeks or even months.
Many billing errors trace back to intake. Wrong policy numbers. Missing NPI codes. Misspelled names. When staff enter data by hand, mistakes happen. Even careful workers miss things when they are rushed.
Digital intake cuts these errors at the source. Patients type their own information. They upload photos of their insurance cards.
The system can check for missing fields before the form is submitted. By the time your billing team sees the data, it is clean and complete.
Clean data means fewer rejected claims. Fewer rejections mean faster payments. Faster payments mean healthier cash flow. For a facility that bills hundreds of claims per month, even a small drop in rejections can mean thousands of dollars.
Let us put numbers to this:
Say, your facility has a 5% claim rejection rate. On average, each rejection costs you $50 in staff time to fix and resubmit. If you process 200 claims per month, that is 10 rejections costing $500.
Drop your rejection rate to 2% with cleaner data, and you save $300 per month, or $3,600 per year. That is real admissions department cost savings that shows up on your books.
Growth is good. But growth brings challenges. More patients mean more intake work. In a paper-based system, the only way to handle more admissions is to hire more staff. This adds salary, benefits, and training costs.
Digital intake breaks this pattern. With the right tools, one admissions coordinator can onboard 3 to 4 patients at the same time. They are not tied to one patient's paper file.
They can monitor multiple digital submissions at once. They can respond to questions by text while forms are in progress.
Think about what this means during a busy week. Your facility gets a surge of calls after a holiday weekend. In a paper-based world, you scramble. Staff work overtime. Some calls go unanswered. Patients go to other facilities.
With digital intake, you scale up smoothly. You send intake links by text. Patients fill out forms on their own time. Your team reviews submissions as they come in. You handle the surge without breaking a sweat.
This kind of scalability is key to long-term growth. It lets you serve more patients without ballooning your payroll. It protects your margins even as you expand. And it supports a stronger Opus EHR ROI over time.
Let us walk through a full example to see how these benefits stack up:
Imagine a facility with 20 admissions per week:
In a paper-based system, they spend an average of 50 minutes per admission on data entry. That is about 17 hours of staff time per week. At $25 per hour, that adds up to $425 per week, or $22,100 per year.
Now, they switch to digital intake:
Data entry time drops to 10 minutes per admission for review and corrections. That is about 3.5 hours per week, or $87.50. The annual cost drops to $4,550. The savings? Over $17,000 per year.
The facility also reduces no-shows by 15% because patients are more committed after completing digital forms. That saves 3 beds per week that would have gone empty. At $500 per day in lost revenue per empty bed, that is $1,500 per week, or $78,000 per year.
Add in billing improvements and storage savings, and the total value can easily exceed $100,000 per year. For a facility looking at addiction treatment admissions ROI, these numbers make a strong case.
Digital intake is not just a nice-to-have. It is a tool that drives real financial results. It supports your team, speeds your billing, and helps you grow without adding headcount. That is what data-driven efficiency looks like in practice.

Every minute your staff spends on paper is a minute they could spend on patients. Every form that gets lost or misread is a risk to your revenue. Every patient who walks out during a long wait is a life you could have changed.
Digital intake for Opus EHR fixes these problems. It moves the boring work off your team's plate. It gives patients a smoother, faster path into care. It creates data that flows cleanly into your systems from day one.
The choice is clear. You can keep doing things the old way and pay the clipboard cost. Or you can make a change that saves time, saves money, and helps more people get the treatment they need.
Your admissions team deserves better tools. Your patients deserve faster access to care. Your facility deserves to see the results in your numbers.
The path forward starts with a single step. Take a look at how digital intake can work for you. Want to see exactly what your facility could save? Use our free ROI calculator to plug in your numbers and get a custom estimate.
How Curogram Simplifies Digital Intake for Opus EHR
Curogram makes digital intake simple for addiction treatment facilities using Opus EHR. The platform connects to your existing system without complex setup. Your team can start seeing results in days, not months.
You create custom intake forms that match your workflow. These forms include all the fields you need, like consent documents, health history, and insurance details.
Patients receive a secure link by text message. They fill out forms on any device, phone, tablet, or computer.
The data syncs with Opus EHR in real time. Your staff can see submissions as they arrive. They can follow up with patients if anything is missing. The whole process happens before the patient ever walks through your door.
Curogram also supports secure two-way texting. This means you can answer patient questions, send reminders, and keep families in the loop. All messages stay HIPAA-compliant. You build trust while you build your census.
The platform helps your admissions team handle more volume. One coordinator can manage multiple patients at once. They spend less time on paperwork and more time on care. This is how you streamline SUD onboarding without burning out your staff.
Facilities using Curogram also report lower no-show rates, faster time to first treatment, and happier staff. The platform is built for behavioral health, so it understands your unique needs. It is not a generic tool forced into your workflow.
If you want to improve your addiction treatment admissions ROI, Curogram gives you the tools to make it happen. The system is easy to learn, fast to deploy, and designed to work with Opus EHR from day one.
Digital intake is not just a tech upgrade. It is a smart business move for any addiction treatment facility using Opus EHR.
The numbers tell the story. You can cut data entry time by up to 80%. You can save 30 to 60 minutes per patient. You can reduce no-shows and AMA departures that drain your revenue. Every one of these gains adds up to real dollars.
But the value goes beyond money. When you remove friction from the intake process, patients start treatment faster. Faster starts mean better outcomes. Better outcomes mean more lives changed.
Your admissions team wins too. They stop being data entry clerks. They get to focus on the human side of their job, talking to families, guiding patients, and building trust. This shift improves morale and reduces burnout.
The path from paper to digital is simpler than you might think. With the right tools, you can make the switch in days. Your staff can learn the system quickly. Patients adapt even faster because they already use their phones for everything.
If you are a facility CEO, CFO, or admissions director, the question is not whether to make this change. It is when. Every week you wait is a week of lost savings. Every month of delay is a month of missed admissions.
Curogram and Opus EHR work together to give you a front door that moves fast and stays compliant. The tools are ready. The ROI is proven. The only thing left is to take action.
Schedule a 10-Minute Demo today to calculate your specific addiction treatment admissions ROI and see how Curogram and Opus EHR can transform your facility's front door.
Transform your facility's front door. Book a demo now to see your specific addiction treatment admissions potential ROI.
Most facilities find that the system pays for itself fast. The break-even point is often within the first 5 to 10 admissions. After that, every benefit goes straight to your bottom line. Think about it this way. If you save $20 in labor per admission and $500 in avoided no-shows each week, your return builds quickly.
Patients who invest effort feel more committed. Filling out forms creates a sense of progress. This psychological investment makes them less likely to skip their scheduled intake.
Digital forms arrive at any time and do not require staff presence. Coordinators can review three to four submissions at once, respond by text, and flag incomplete items without being tied to one file.

💡 Behavioral health clinical texting helps addiction treatment centers convert more leads into admissions by enabling instant, secure communication...
💡 Clinics using Osmind can boost their Osmind onboarding ROI by switching to digital intake. This cuts the time from first inquiry to the first...
💡 Digital patient intake for Opus EHR helps addiction treatment and behavioral health clinics speed up admissions and reduce paperwork. Patients...