How to Reduce Data Entry Errors in Prime Clinical | Clean Intake Data
💡 You can reduce data entry errors in Prime Clinical Intellect by removing manual transcription from your intake process.When staff retype data...
11 min read
.jpg) Mira Gwehn Revilla
:
February 19, 2026
Mira Gwehn Revilla
:
February 19, 2026

A single wrong digit in a member ID can hold up thousands of dollars for weeks. That one typo, punched in by a rushed front desk staffer, turns into a denied claim that your billing team has to chase down. It is a small mistake with a big price tag.
For practices that use CollaborateMD, this problem hits close to home. The system is built to process claims fast, but it can only work with the data it receives.
When that data is wrong, even the best billing module cannot save you. The result is a growing pile of "Member Not Found" denials that drain time, money, and morale.
Here is the hard truth: Most denied claims are not caused by tricky payer rules or complex codes. They are caused by simple data entry errors made at the front desk.
A misspelled last name. A birth date with the wrong year. An insurance ID with one flipped number. These are the mistakes that keep your revenue stuck in limbo.
The good news is that these errors are also the easiest to prevent. You do not need to hire more staff or add another layer of review. You need to change how patient data gets into your system in the first place.
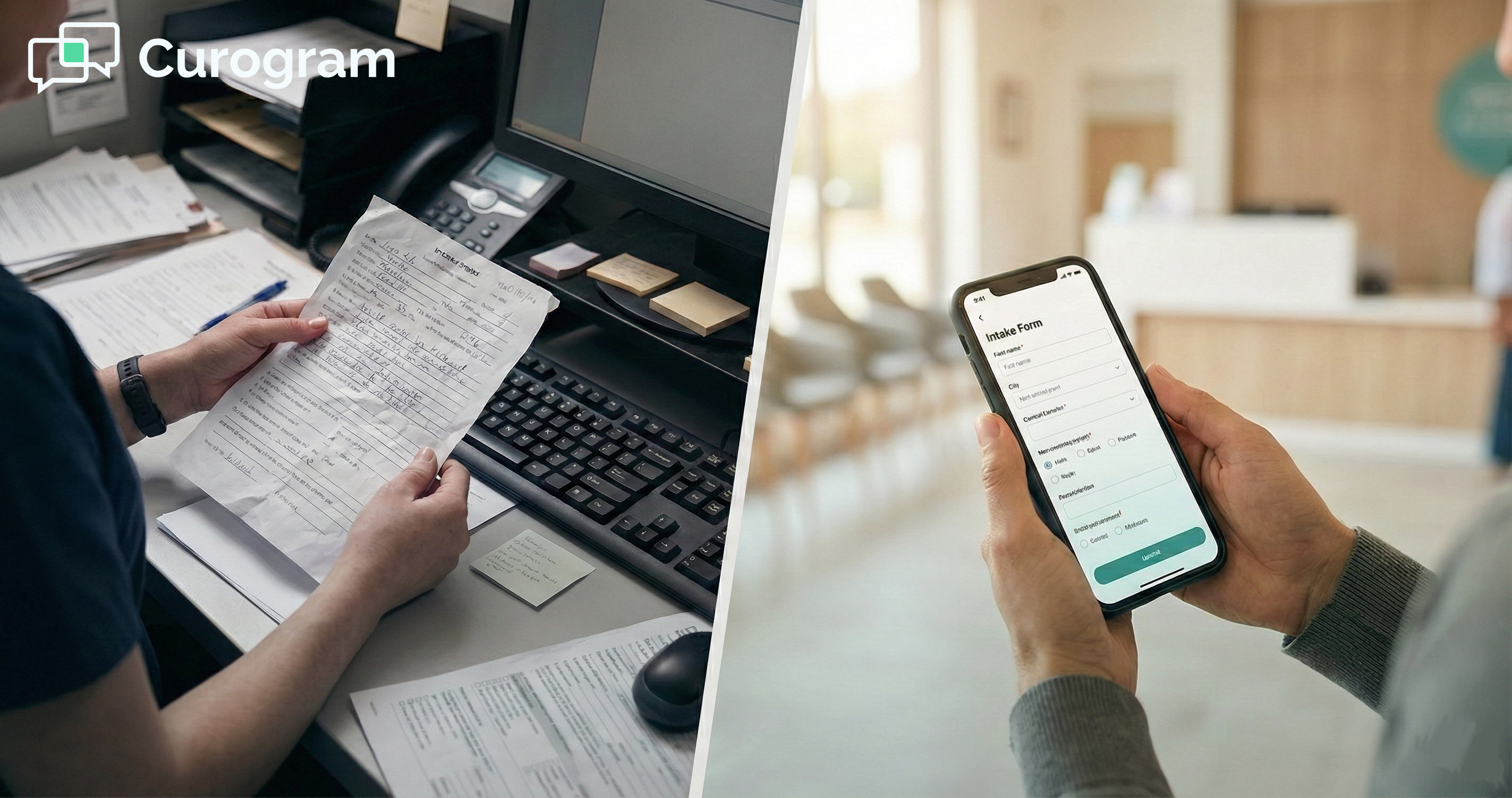
Digital intake forms let patients type in their own details on their phones before they arrive. The data flows right into CollaborateMD without anyone at the front desk touching it. No clipboard. No handwriting to decode. No re-keying from a paper form.
This article breaks down why manual entry is the root cause of most claim denials. It shows you exactly how digital intake solves the problem. It walks through the real money you stand to gain when you reduce claim denials in CollaborateMD using a source-verified data approach.
Every medical practice knows the sting of a denied claim. But few stop to ask where the problem really starts. In most cases, it starts at the front desk, with a pen, a clipboard, and a staff member who is juggling five tasks at once.
Manual data entry has a known error rate of 1% to 3%. That might sound small. But for a practice that files 500 claims a week, that means 5 to 15 claims go out with bad data every single week. Over a month, you are looking at 20 to 60 claims that will bounce back before a payer even looks at the clinical side.
|
Think about what that means in dollar terms: Say, your average claim is worth $150. At just a 2% error rate on 500 weekly claims, that is 10 claims denied per week. That adds up to $1,500 a week in delayed or lost revenue. Over a year, that is more than $78,000 sitting in limbo, all because of typos. |
The most common denial tied to data entry is the "Member Not Found" code. This denial does not mean the patient lacks insurance.
It means the system could not match the claim to the patient's record at the payer. The usual cause is simple: a wrong member ID number, a misspelled name, or a birth date that does not match what the payer has on file.
These are not clinical errors. They are clerical errors. And they cost at least $25 each to rework, according to industry research.
That cost covers the time your billing staff spends to find the mistake, call the payer, correct the claim, and resubmit it. For a busy practice, that rework time adds up fast.
Here is the part that makes it worse: The billing team in the back office is not the one making these mistakes. They are cleaning up messes made by the front desk.
Front desk staff are often rushed, short-staffed, and dealing with a full waiting room. They are copying data from smudged paper forms or trying to read a patient's handwriting.
CollaborateMD patient registration errors like these are almost built into the process when you rely on manual entry.
|
Now, picture a real scenario: A patient named "Joanne" writes her name on a paper form. The front desk staffer reads it as "Joanna" and keys it in. The claim goes out with the wrong name. The payer's system does not find a match. The claim is denied. Three weeks later, a biller catches it, fixes the name, and resubmits. The practice waits another 14 to 30 days for payment. One letter cost the practice six weeks of cash flow. |
This is not a rare event. It happens in practices every single day. And it does not just affect revenue. It affects trust between departments.
Billing staff get frustrated with the front desk. Front desk staff feel blamed for something they barely had time to do right. The whole cycle creates tension that no staff meeting can fix.
The root problem is not the people. It is the process. When you ask humans to hand-key data from paper forms under time pressure, errors are not a risk. They are a guarantee. The only way to fix it is to remove that step from the process entirely.
If the problem is bad data going into CollaborateMD, the fix is simple. Let the patient enter the data themselves.
This is the idea behind source-verified data injection. Instead of a front desk staffer copying info from a paper form, the patient fills out a digital form on their own phone or device.
They know their name. They know their birth date. They know the spelling of their street address. And with auto-fill on their phone, much of the data comes in with standard formatting already applied.
Think about it. You would never ask a stranger to type your email address for you. So why ask a stranger to type a patient's 12-digit insurance member ID from a blurry photocopy?
Patient self-entry is the first layer of defense against bad data. But it is not the only one. The second layer is OCR, or optical character recognition.
|
Here is how it works: The patient opens the digital form on their phone and snaps a photo of the front and back of their insurance card. The OCR tool reads the text on the card and pulls out the key fields: member ID, group number, payer name, and plan type. |
This step matters because even careful patients can make a mistake when typing a long string of numbers. OCR takes the guesswork out. It reads the card the same way a scanner reads a barcode. The chance of error drops from 1% to 3% down to a fraction of a percent.
Now, here is where the real value shows up for CollaborateMD users. The data from these digital forms does not just land in a PDF or sit in an inbox. It feeds right into the patient record inside CollaborateMD.
The name, birth date, address, and insurance fields all map to the right spots in the PM module. Your biller opens the record and sees the data already in place, ready to review and approve.
This is what makes it different from just emailing a form to the patient. A PDF still needs to be read and re-keyed by a human. A truly connected digital form skips that step. It acts like a bridge between the patient's phone and your billing system.
The process also supports automated insurance verification. Once the patient's payer info is in the system, the practice can run an eligibility check right away, before the visit even starts.
This means you can catch expired plans, wrong group numbers, or inactive policies before the patient walks through the door. No surprises at the time of billing.
For practices focused on medical billing data accuracy, this workflow is a game changer. You go from a model where data is entered once by a staffer and never checked, to a model where data is entered by the patient, scanned by OCR, and verified by the system. Three layers of checks, with no extra staff needed.
|
Let us go back to the "Joanne" example from the last section: With digital intake, Joanne types her own name. Her phone auto-fills her address. She snaps a photo of her insurance card, and OCR pulls the member ID. The data flows into CollaborateMD. The biller reviews it and submits the claim. No typo. No denial. Payment in 14 to 30 days. |
That is what source-verified data injection looks like in practice. It does not add steps. It removes the step that causes the most damage.

The goal of every billing team is simple: get the claim paid on the first try. In billing terms, this is called First-Pass Yield, or FPY. It measures the share of claims that are paid without any rework, resubmission, or appeal. The higher your FPY, the faster your cash comes in.
For most practices, the average FPY sits around 80% to 85%. That means 15% to 20% of claims need extra work before they get paid. Some of those are complex clinical denials. But a large chunk are simple data errors that should have never happened in the first place.
When you clean up the data going into CollaborateMD, you directly improve clean claim rate. Clean claims are those that pass all edits and checks the first time they are sent. They do not trigger payer rejections. They do not sit in a denial queue. They move straight through the pipeline and get paid.
|
Let us put numbers to this: Say, your practice submits 2,000 claims per month. At an 80% FPY, 400 of those claims get denied or rejected. If even half of those denials are due to data errors, that is 200 claims per month that could have been clean. |
Now, imagine you use digital intake to cut those data-related denials by 75%. That is 150 claims per month that now go through clean on the first pass.
At an average claim value of $150, that is $22,500 per month in revenue that no longer sits in denial limbo. Over a year, that adds up to $270,000 in faster cash flow.
The speed difference is real. A clean claim is paid in 14 to 30 days. A denied claim takes 45 to 90 days. That gap matters for any practice trying to manage payroll, rent, and supplies. When your Days Sales Outstanding drops, you have more cash on hand for the things that keep the doors open.
There is also the staff time you get back. Think about what happens when a claim is denied for a data error. A biller has to pull up the claim. They have to figure out what went wrong.
They call the payer or log into the portal to check the details. They fix the data in the patient record. They resubmit the claim. Then they wait again.
That process takes 15 to 30 minutes per claim. If your billing team is fixing 200 data-related denials a month, that is 50 to 100 hours per month spent on rework. That is more than half a full-time employee doing nothing but fixing typos.
Now, picture what that staffer could do with those hours back. They could work on high-value denials that need clinical review. They could follow up on aged claims worth $5,000 or more. They could handle prior authorization appeals that require real expertise. Instead, they are fixing a misspelled last name for the third time this week.
Want to know exactly how much those lost hours cost your practice? Curogram's ROI Calculator for staff efficiency lets you plug in your monthly volume, time per task, and labor cost to see the real number. Practices that automate routine tasks with Curogram have cut up to 90% of that manual work.

When you reduce claim denials in CollaborateMD using digital intake, you are not just saving money. You are freeing up your most skilled staff to do the work that only they can do.
|
Atlas Medical Center saw this play out in real terms: After switching to digital intake forms that synced with their billing system, they saw a sharp drop in errors tied to data entry. The result was a clear lift in monthly revenue, not because they saw more patients, but because more of their claims went through clean the first time. |
Here is another angle most practices miss: the cost of write-offs. Not every denied claim gets reworked. Some fall through the cracks. A biller gets busy. The filing deadline passes. The claim is written off.
For practices with high denial rates, write-offs can quietly eat 3% to 5% of total revenue. That is money you earned but will never collect, all because of a data error that could have been prevented.
Digital intake also helps on the patient side. When patients fill out their own forms ahead of time, they are more likely to double-check their own info. They can pull out their insurance card and type the numbers directly.
This calm, focused data entry leads to better medical billing data accuracy across the board. And when the data is right from the start, every step after it gets easier: eligibility checks, claim submission, payment posting, and follow-up.
You cannot fix a billing process that starts with bad data. No matter how skilled your billing team is, they cannot make a clean claim out of a wrong member ID or a misspelled name. The error has to be stopped before it enters the system.
That is what digital intake does. It moves data entry away from rushed front desk staff and puts it in the hands of the patient. The person who knows their own info best is the one typing it in.
This is not about looking modern or going paperless for the sake of it. This is about getting paid for the work your providers have already done.
Every claim that goes out clean is revenue that comes back faster. Every denial you prevent is time your billing team gets back.
For CollaborateMD users, the fit is natural. Digital forms feed data right into the fields your billers already use.
The math is clear. Fewer typos mean fewer denials. Fewer denials mean faster payments. Faster payments mean better cash flow. And better cash flow means a practice that can grow, invest, and take care of its team.
Clean claim rate improvement does not require a full system overhaul. It starts with one change: how you collect patient data at the front door.
Why Curogram Is the Easiest Fix for Front Desk Data Errors
Curogram connects the gap between your patients and your CollaborateMD billing system. When a patient books a visit, your office sends them a text with a link to a digital intake form.
The patient opens it on their phone and fills in their name, birth date, address, and insurance details. They can also snap a photo of their insurance card, and OCR reads the key fields from the image.
The data from the form goes straight into the patient record in CollaborateMD. It maps to the right fields, so your billing team does not have to re-enter anything. They just review, approve, and submit the claim.
Curogram is HIPAA-compliant, so patient data stays safe from the moment it leaves the phone to the moment it lands in your PM system. No paper trail. No unsecured emails. No faxes sitting on a counter.
The system also helps with automated insurance verification. Once the payer details are in the record, your team can check eligibility right away. If a plan is expired or a group number is wrong, you catch it before the visit, not after the claim is denied.
For practices that deal with CollaborateMD patient registration errors on a daily basis, Curogram removes the root cause. It takes data entry out of the hands of busy front desk staff and gives it to the one person who knows the info best: the patient.
The result is better medical billing data accuracy, fewer denials, and faster payments. All with less work for your team.
Curogram works as a simple add-on to CollaborateMD. Setup is fast, training is minimal, and the impact on your clean claim rate shows up quickly.
Claim denials cost your practice time, money, and momentum. But the biggest source of those denials is also the most fixable. Simple data entry mistakes at the front desk cause a huge share of rejections that your billing team has to clean up later.
The answer is not working harder. It is working smarter at the point where data enters your system. When patients fill out their own details on a digital form, the typos that trigger "Member Not Found" denials stop happening.
When OCR scans the insurance card, long member IDs come through right every time. When the data syncs straight to CollaborateMD, there is nothing left to re-key.
This is not a big system change. It is one shift in how you collect patient data. And it touches everything downstream: your clean claim rate, your days to payment, your billing team's workload, and your monthly cash flow.
Practices that make this switch see the results fast. More claims paid on the first pass. Fewer hours spent on rework. Less revenue lost to write-offs. And a billing team that finally has time to focus on the work that matters most.
You already do the hard work of caring for patients every day. Your revenue should not get stuck because of a wrong digit or a misspelled name.
Take the first step toward fewer denials and faster payments. [Get a Demo] to see how Curogram's digital intake forms help you reduce claim denials in CollaborateMD and keep your revenue moving.
Take the first step toward fewer denials and faster payments. Book a demo with us to see how Curogram's digital intake forms keep your revenue moving.
Each one costs at least $25 in staff time to rework, plus 30 to 60 extra days before payment arrives. For a practice with dozens of these per month, the total loss in time and cash flow adds up fast.
Patients fill out their forms on their phones before the visit. Front desk staff no longer hand-key data from paper forms. Their role shifts from data entry to review and check-in, which saves time and reduces stress.
Preventing a denial costs almost nothing. Fixing one costs $25 or more and takes weeks. Focusing on clean data up front saves more money and staff hours than chasing denials after they happen.
💡 You can reduce data entry errors in Prime Clinical Intellect by removing manual transcription from your intake process.When staff retype data...

💡 Secure patient intake for CollaborateMD helps billing teams cut claim denials by removing manual data entry errors at the front door. Patients...
💡 Using 2-way texting to verify patient details helps CollaborateMD users fix "unclean" claims before they go out, cutting denial rates tied to...