Simplifying Virtual Visits in Veradigm with Telehealth
💡 Telehealth helps imaging centers work faster and smarter. Virtual visits that Veradigm users rely on cut down delays and improve patient care....
16 min read
.jpg) Mira Gwehn Revilla
:
Updated on January 9, 2026
Mira Gwehn Revilla
:
Updated on January 9, 2026
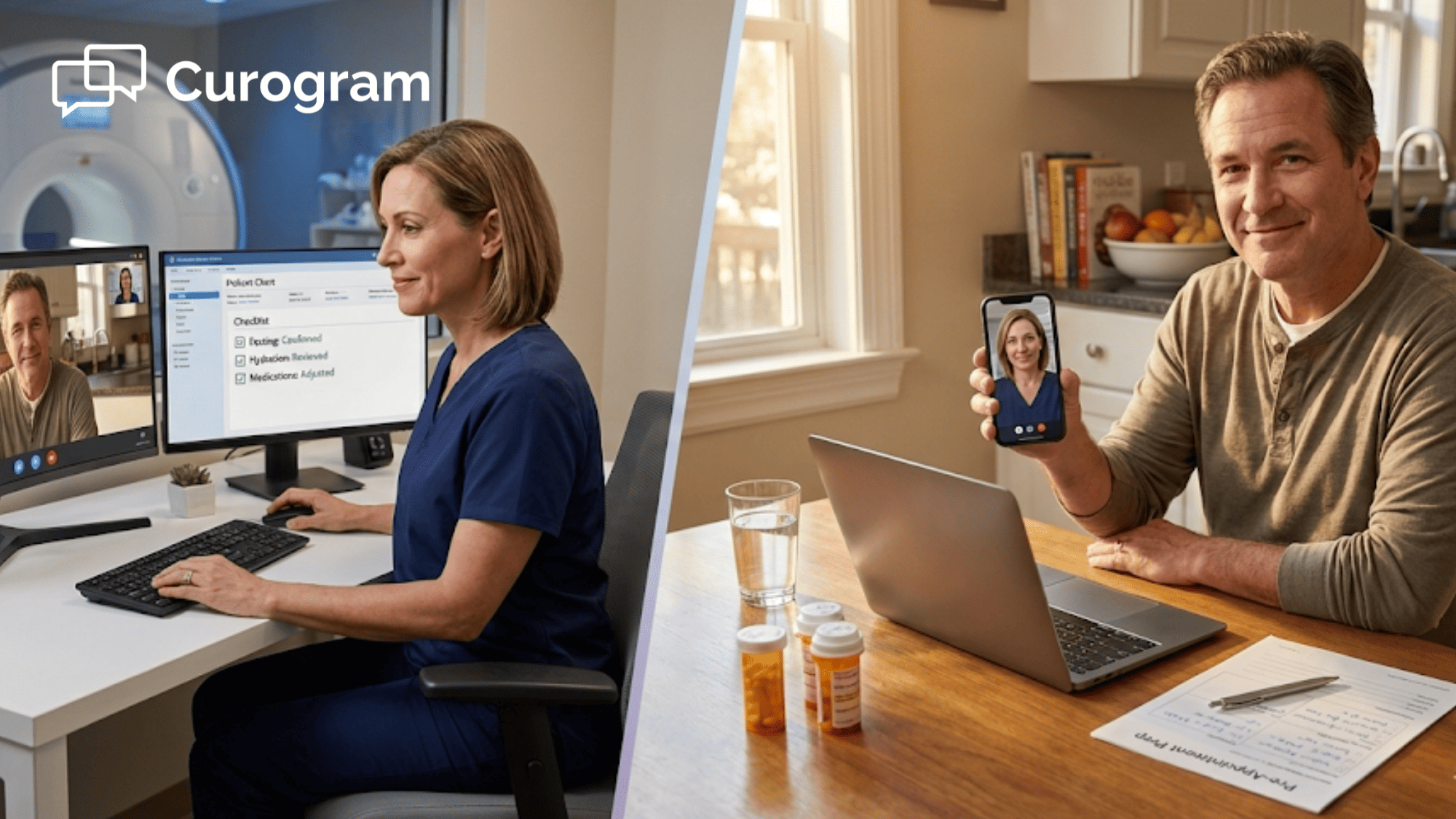
Table of Contents
A patient shows up for an MRI. They ate breakfast. The scan gets canceled.
This happens more than you think. Prep mistakes waste time, money, and scanner slots. Patients leave upset. Staff scramble to fill the gap.
Radiology, vascular, and IR teams face this daily. Phone lines stay jammed with simple questions. Patients forget rules they heard once on a call two weeks ago. And front desk staff spend hours fixing issues that could have been avoided.
Virtual visits offer a smarter path. With StreamlineMD, imaging centers now use telehealth to prep patients before they arrive. A quick video chat or text exchange confirms the details that matter most. Did the patient stop eating? Are there metal implants? Did they hold the right meds?
These are not complex cases. But they need clear answers. When you get those answers early, the schedule runs smoother.
This shift helps more than radiology. Vascular labs and IR suites see the same gains. A five-minute remote consult can catch a safety issue that would have delayed a case by hours.
The result? Fewer no-shows. Fewer incomplete exams. Less stress on staff.
Virtual visits through StreamlineMD also support post-treatment follow-ups. Patients who just had an IR procedure can check in from home. Nurses can spot problems early. And patients feel cared for without a long drive.
Curogram powers the texting and video tools that make this work. Together, these platforms create a seamless patient experience from booking to recovery.
In this guide, you will learn how imaging centers use telehealth across their daily workflows. We will cover prep, screening, follow-up, and more. Let's dig in.
Imaging centers run on tight schedules. One missed detail can throw off an entire day. The root cause is often poor prep. Patients receive instructions, but those instructions get lost, ignored, or confused. Without telehealth integration, it's too late to fix the problem by the time the patient arrives.
MRI, CT, and ultrasound exams each have their own rules. Some need fasting. Others require contrast dye or a full bladder. A few demand that patients stop certain meds.
Most centers share these rules over the phone. A staff member reads from a script. The patient listens, says "okay," and hangs up. Two weeks later, that patient eats toast before their abdominal MRI.
The scan has to be rescheduled. The slot stays empty. The next patient waits longer. This cycle repeats across radiology, vascular, and IR settings. And every repeat costs time, revenue, and trust.
Vascular and IR procedures carry higher stakes. These are not simple scans. Patients may need sedation, arterial access, or drug infusions.
That means more screening. Staff must confirm blood thinners, insulin use, allergy history, and kidney function. A single gap can force a same-day cancel.
For example, a patient on warfarin may need to stop the drug five days before a procedure. If no one verifies this, the case gets pushed. The patient is upset. The care team loses a slot that took weeks to book.
Phone calls alone cannot track all these details. Staff are busy. Patients forget to mention things. Notes get lost between systems.
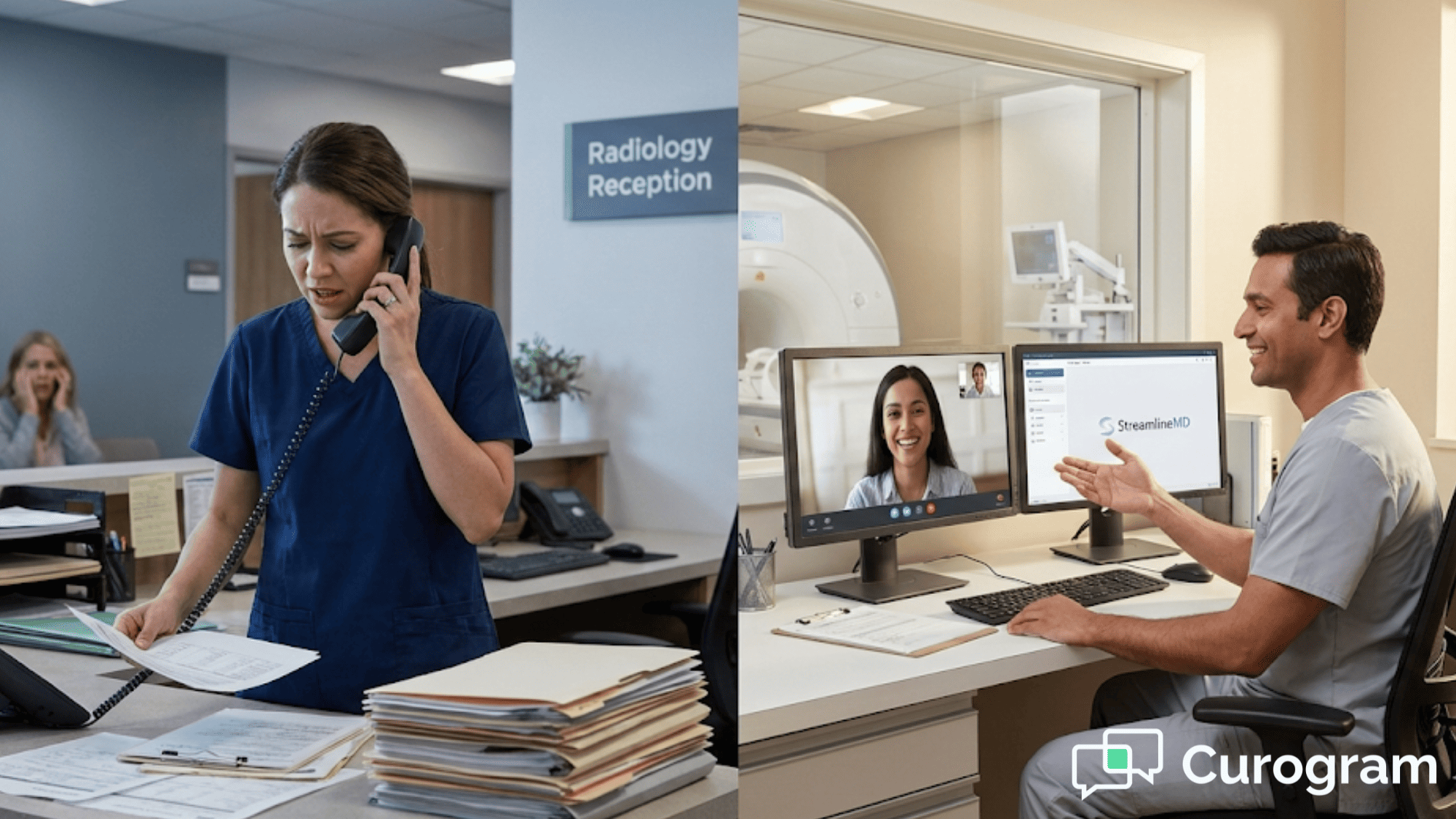
Front desk teams handle dozens of calls each day. Many of those calls are simple prep questions. "Can I drink water?" "What time do I stop eating?" "Do I need a ride home?"
Each call takes time. Staff must pull up the patient chart, find the procedure type, and look up the rules. Then they explain the same thing they explained to three other patients that morning.
This ties up phone lines. Other patients wait on hold. Urgent calls get delayed. Staff feel burned out by the end of the day.
The problem grows in multi-site networks. Each location may give slightly different answers. Patients get confused. Mistakes increase.
A large imaging group may have ten or more sites. Each site has its own staff, workflows, and habits. Without a shared system, prep messages vary. One site may send a text reminder. Another may rely on a phone script. A third may just mail a letter.
Patients who visit more than one site notice these gaps. Trust drops. Errors rise. Remote consultations can fix this. When every site uses the same virtual visit tools, patients get the same message no matter where they go.
Every call, reschedule, and fix-it task takes time away from patient care. Staff could be helping with check-in, imaging, or recovery. Instead, they are on the phone explaining why the patient cannot wear jewelry in the MRI suite.
The real cost is not just minutes. It's morale. Burned-out staff leave. Turnover rises. Training costs climb.
Telehealth helps by moving these tasks off the phone. A short video consult or text chat handles the basics. Staff can focus on the patients who need hands-on help.
Telehealth is not just for sick visits. It is a prep tool. Imaging centers now use virtual visits to make sure patients are ready before they walk through the door. This approach cuts delays, fills schedule gaps, and keeps scanners running on time.
A virtual prep consult takes five to ten minutes. A staff member connects with the patient over video or secure text. They review the key details for that patient's exam.
For MRI, this means confirming that the patient has no metal implants, pacemakers, or shrapnel. It also means checking for claustrophobia. A patient who panics in the scanner wastes everyone's time.
For CT, the consult confirms kidney function and allergy status. Contrast dye can harm patients with poor kidney health. A quick check avoids a dangerous situation.
For ultrasound, the consult confirms fasting or hydration rules. A pelvic ultrasound needs a full bladder. An abdominal ultrasound needs an empty stomach.
These checks are simple. But they prevent incomplete studies. When a study is incomplete, the patient must come back. The reading is delayed. The referring doctor waits. Care slows down.
Virtual visits through StreamlineMD flag these issues early. If a patient has a new pacemaker, the team can adjust the plan before the patient drives an hour to the center.
Patients have questions. That is normal. But not every question needs a phone call.
With secure texting, patients can send a quick message. "Can I take my morning pills?" The response comes in minutes, not hours. The patient knows the answer. The phone line stays open.
This real-time exchange replaces the old model of endless voicemails and callbacks. Staff can handle multiple chats at once. Patients get faster answers.
For example, a patient scheduled for a contrast CT might text, "I have shellfish allergy. Is that a problem?" The team can reply right away with the right next step. This kind of remote consultation builds trust. Patients feel heard. Staff feel less rushed.
When patients arrive ready, the schedule holds. Technologists start scans on time. The waiting room does not back up.
This matters most for high-volume modalities. An MRI suite with only two scanners cannot afford gaps. A single no-show or delay can cascade into late nights and overtime.
Virtual prep visits help by catching problems before the appointment day. If a patient cannot fast, staff know in advance. They can reschedule early. The slot gets filled by another patient who is ready.
Over time, this creates a more stable rhythm. Staff know what to expect. Patients move through the system without friction.
Consider this:
A busy outpatient imaging center run six MRI slots each morning. Without virtual prep, two of those slots might fail due to poor prep. With virtual prep, that number drops to one or zero.
That one saved slot adds up. Over a month, it could mean dozens of extra completed scans. Over a year, it could mean thousands of dollars in recaptured revenue.
Virtual visits also help with add-on exams. If a patient needs both an MRI and an ultrasound, staff can confirm prep for both exams in one chat.
The result is a tighter workflow. Less waste. More throughput. And happier patients who feel supported from the moment they book.

Vascular and IR procedures demand more than standard imaging. They involve sedation, access sites, and recovery time. Patients need careful screening before the day of the case.
Telehealth helps teams manage this screening without adding more in-person visits. It keeps patients informed and catches risks early.
Blood thinners are common. Millions of patients take them for heart, stroke, or clot risks. But these drugs create problems before IR and vascular procedures. A patient on aspirin may be fine for some cases. A patient on warfarin or a newer blood thinner may need to stop the drug days before.
The challenge is tracking who takes what. Patients often forget to mention all their meds. Some take supplements that also thin blood, like fish oil or vitamin E.
Virtual visits give teams a chance to review the full list. A nurse can ask direct questions. The patient can show their pill bottles on video.
This kind of screening catches gaps that phone calls miss. The visual check adds a layer of safety. Staff can see the label and verify the dose.
For example, a patient scheduled for a liver biopsy might be on Eliquis. The team needs to know the last dose. A virtual visit lets them confirm this detail and explain when to restart the drug after the procedure.
If the patient has not stopped the drug in time, the team can reschedule before the patient travels to the center. This avoids a wasted trip and a frustrated patient.
Virtual screening also helps with insulin and diabetes management. Some procedures require fasting. Fasting with insulin can cause low blood sugar. A pre-procedure consult lets the team adjust the insulin plan.
Consent forms are not just signatures. They are conversations. Patients need to understand what will happen, what the risks are, and what to expect after.
In the past, this happened in person, often minutes before the procedure. Patients felt rushed. Doctors felt pressed for time. Consent became a checkbox instead of a true discussion.
Telehealth changes this. Teams can walk patients through consent over video days before the case. The patient has time to ask questions. The doctor has time to explain. This builds trust. A patient who understands the plan is less anxious on procedure day. They follow prep rules better. They know what to do at home after.
For example:
A patient booked for a uterine fibroid treatment can review the consent form during a virtual visit. The interventional radiologist explains the steps. The patient asks about recovery time. Both sides feel confident moving forward.
Pre-procedural instructions also benefit from this approach. IR cases often have long prep lists. NPO rules, bowel prep, medication holds, and arrival times all need to be clear.
A virtual visit lets staff walk through each item. They can send follow-up texts with written reminders. Patients have a record to refer back to.
This reduces same-day confusion. Patients arrive ready. Staff do not need to repeat instructions in the holding area.
Complex IR cases involve more than one team. Schedulers book the room. Nurses prep the patient. Technologists run the equipment. Anesthesia may be involved.
When these teams do not talk, problems arise. The patient shows up, but anesthesia was never booked. The room is ready, but the implant was not ordered.
Telehealth helps by creating a shared touchpoint. The pre-procedure virtual visit becomes a checkpoint. If something is missing, it gets flagged before the day of the case.
For example, a patient scheduled for a port placement needs lab work. The virtual visit confirms the labs were drawn. If not, staff can order the labs and reschedule the case. This kind of proactive work saves hours of scrambling. It also protects the patient from unsafe situations.
Multi-site IR practices see even more benefit. A patient at one location may need to travel to another for a specialized procedure. Virtual visits keep the information flowing between sites.
Consider this:
A vascular group has three locations. A patient sees a doctor at Site A. The procedure happens at Site B. Post-treatment follow-ups occur at Site C. Without a shared system, details get lost.
Virtual visits through StreamlineMD link these sites. Each team can see the same notes. The patient gets the same message no matter who they talk to.
Same-day cancellations hurt everyone. The patient loses time. The team loses revenue. The schedule falls apart.
Most same-day cancels could have been avoided. The patient ate when they should have fasted. The blood thinner was not stopped. The ride home was not arranged.
Virtual screening catches these issues early. A quick video chat two or three days before the case confirms everything is in order.
If something is wrong, staff have time to fix it. They can reschedule the case to a new slot instead of leaving the original slot empty.
This approach also reduces patient no-shows. A patient who has a pre-procedure consult feels more connected to the care team. They are less likely to forget the appointment or skip it due to fear.
IR and vascular procedures can feel scary. Patients may not understand what an interventional radiologist does. They may picture open surgery instead of a small needle puncture.
A virtual visit gives the team a chance to explain. A quick video chat can show the patient what to expect. The radiologist can describe the steps in plain terms.
This calms nerves. A relaxed patient is easier to prep, easier to sedate, and easier to recover.
Remote consultations also let patients bring family members into the conversation. A spouse or adult child can join the video call. They hear the same information. They can help the patient follow the prep rules.
This kind of support matters. It leads to better outcomes and higher satisfaction scores.
Phones ring all day at imaging centers. Staff answer the same questions over and over. This drains time and energy. Telehealth shifts these tasks to more efficient channels. The result is less burnout and better service.
Most patient calls are simple. "What time is my scan?" "Do I need to fast?" "Where do I park?"
These questions do not need a live phone call. A text or video message can handle them just as well.
With virtual visits through StreamlineMD, staff can send prep reminders by text. Patients reply with questions. Staff answer in a few taps. No hold time. No voicemail tag.
This frees up phone lines for urgent calls. A patient with a billing issue or a referring doctor with a stat request can get through faster.
The shift also improves accuracy. A written text gives the patient a record. They can refer back to it instead of relying on memory.
Call centers at large imaging networks see the biggest gains. A single text thread can replace three or four phone calls. Staff handle more patients in less time.
A phone call is one-to-one. A staff member talks to one patient until the call ends.
Text messaging is different. One staff member can manage five or ten chats at once. They check each thread, type a reply, and move to the next.
This boosts productivity without adding headcount. The same team handles more volume.
For example, a front desk team of three might take 90 calls a day. With texting, they can handle 150 patient contacts in the same time.
The key is asynchronous flow. Patients send a message when it fits their schedule. Staff reply when they have a moment. No one waits on hold.
Large imaging groups often struggle with message drift. One site sends one version of the prep rules. Another site sends something slightly different.
This causes confusion. Patients who visit more than one site notice the gaps.
Virtual visit tools solve this by using shared scripts and templates. Every site sends the same text. Every video consult follows the same checklist.
This creates a unified patient experience. Trust grows. Mistakes shrink. Managers can also track performance across sites. They can see which locations have higher reschedule rates. They can identify coaching needs.
Recovery does not end at discharge. Patients need guidance after they leave the center. Telehealth makes follow-up easy and fast.
Patients often worry after an IR procedure. Is the bruise normal? Should the site still hurt? When can I shower? Without guidance, some patients go to the ER. They wait hours for reassurance that everything is fine.
A quick post-treatment follow-up by video or text can prevent this. A nurse checks in the next day. The patient shares a photo of the site. The nurse confirms all looks good. This saves the patient time and stress. It also saves the health system money.
A follow-up message shows the patient they are not alone. The care team is still there. This simple gesture builds loyalty and trust.
IR and vascular cases can feel scary. Patients go home with puncture sites, bandages, and a list of warning signs. Many feel nervous once they leave the center. They wonder if they are healing right.
A text the next morning changes that. Even a short message like "How are you feeling today?" makes a big impact. It tells the patient someone is watching over them.
Patients who feel supported are more likely to return for future care. They also tell friends and family about their good experience. This word-of-mouth matters for your reputation.
Follow-up messages also give patients a chance to ask small questions. Instead of calling the office or worrying in silence, they can reply to the text. The nurse responds. The patient feels heard.
Sometimes, the bruise is not normal. Sometimes the pain is a warning sign. Virtual follow-up lets nurses spot these issues early. If something looks wrong, they can bring the patient back quickly.
Consider a patient who had a femoral artery access for an IR procedure. The next day, they notice swelling near the groin. Without follow-up, they might wait to see if it goes away. By the time they act, a small hematoma could grow into a bigger problem.
With a virtual check-in, the nurse asks for a photo. The patient snaps a quick image and sends it. The nurse sees the swelling and asks more questions. Within an hour, the patient is back at the center for a quick exam.
This early catch can prevent a small problem from becoming a big one. It can avoid a hospital admission, emergency surgery, or worse.
Virtual follow-up also helps track trends. If several patients report the same issue, the team can review their technique or discharge instructions. This feedback loop improves care for everyone.
Nurses can also use follow-up chats to reinforce home care. Remind the patient to keep the site clean. Confirm when they can resume normal activity. Answer questions about medications.
Patients expect modern service. They book flights on apps. They order food with a tap. Healthcare should feel just as simple. Virtual visits through StreamlineMD meet this need.
No one likes waiting. A quick text with clear prep rules beats a callback that never comes. Timely messages reduce anxiety. Patients know what to do. They feel in control.
This matters most for first-time patients. A first MRI can feel scary. The machine is loud. The space is tight. A simple message explaining the process helps calm nerves.
Think about what patients go through. They book a scan weeks in advance. They forget the prep rules by day two. Then they wait for a call that may or may not come. By the time they remember to ask a question, the office is closed.
Virtual communication fixes this gap. A text arrives with clear steps. The patient reads it on their own time. They can reply with questions right away. No hold music. No missed calls.
This flow builds confidence. Patients arrive knowing what to expect. They trust the process. They trust your team. And that trust starts with one simple, timely message.
IR patients face bigger procedures. A port placement or tumor ablation is not routine. These patients need extra support. Easy access to the care team builds trust. A patient who can text a question at 8 PM feels cared for.
Satisfaction scores rise when patients feel heard. High-acuity cases come with high emotions. Patients may be dealing with cancer, chronic pain, or failing organs. They carry stress into every interaction. Small frustrations feel bigger when the stakes are high.
A missed callback can feel like neglect. A confusing voicemail can spark panic. These patients need more than standard service. They need to feel like someone is paying attention.
Virtual access gives them that lifeline. When a patient can send a quick text after hours, they feel connected. Even if the nurse replies the next morning, the patient knows their message was received.
This sense of access changes the entire experience. Patients rate their care higher. They leave better reviews. They refer friends and family. For IR practices, this can mean stronger patient loyalty and a better reputation in the community.
Telehealth removes barriers. Patients do not need to call during office hours. They do not need to drive in for a quick question. This convenience matters for busy families and working adults. It also helps patients in rural areas who live far from the center.
A modern experience keeps patients coming back. It also sets your center apart from the competition. Today's patients compare healthcare to every other service they use. They expect fast replies. They expect digital options. When a practice still relies only on phone calls and paper forms, it feels outdated.
Virtual visits signal that your center keeps up with the times. A patient who can prep for their scan via text feels respected. A patient who can ask a post-procedure question from their couch feels valued.
This convenience also reduces no-shows. Patients who feel engaged are less likely to skip appointments. They remember the prep rules. They show up ready.
For imaging centers, this modern approach is no longer optional. Patients have choices. They will go where the experience is easiest. Virtual support helps you win that choice every time.
Telehealth is just one piece of the puzzle. Other tools work alongside it to improve daily operations.
Practices using StreamlineMD and Curogram can also benefit from HIPAA-compliant texting for secure patient messages. Mass texting helps send prep reminders to dozens of patients at once. Appointment reminders cut no-show rates by alerting patients before their visit.
Reputation management tools ask happy patients to leave reviews. This boosts your online presence.
Online patient forms let patients fill out paperwork from home. No clipboards. No long waits.
Text-to-Pay makes billing easy. Patients get a link. They tap to pay. Collections improve.
Together, these tools create a full system for patient engagement. Each piece supports the others.
How Curogram Powers Telehealth for StreamlineMD Practices
Curogram is the engine behind seamless patient communication. It connects the dots between texting, video, and workflow tools.
For imaging centers, Curogram offers HIPAA-compliant two-way texting. Patients can ask questions without calling. Staff can reply from one central dashboard.
The platform also supports video visits. A nurse can launch a virtual consult with a single link. No app download needed. Patients click and connect.
This simplicity matters. A patient who struggles with tech will not show up for a video call that requires three logins. Curogram removes that barrier.
Integration with EMRs is another key feature. Staff do not need to enter data twice. The system syncs with existing records.
Automated reminders reduce manual work. Staff set the rules once. The system sends texts on schedule.
For multi-site practices, Curogram offers shared templates. Every location uses the same scripts. Patients get the same message no matter where they go.
Curogram also tracks results. Managers can see open rates, response times, and reschedule trends. This data helps teams improve.
The platform reduces phone call volume by up to 50%. Staff productivity rises by 30% or more. Patients get faster answers. Everyone wins.
When paired with StreamlineMD, Curogram creates a modern, patient-friendly layer for radiology, vascular, and IR practices. It handles the small tasks so staff can focus on care.
If your imaging center still relies on phone calls and paper forms, you are falling behind. Curogram brings your workflow into the current era.
Imaging centers face real pressure. Schedules are tight. Patients arrive unprepared. Staff juggle too many calls.
Telehealth offers a clear path forward. Virtual visits through StreamlineMD help radiology, vascular, and IR teams work smarter.
Prep consults catch problems before they cause delays. A quick video chat confirms fasting, implants, and medication holds. The scanner runs on time. The schedule stays full.
Pre-procedure screening protects patients and staff. Blood thinner checks happen early. Consent discussions happen at home, not in the holding area. Patients feel informed and calm.
Post-treatment follow-ups keep patients connected. A nurse can check in by text the next day. Small worries get answered fast. Big problems get caught early.
Call centers see relief, too. Remote consultations and texting move simple questions off the phone. Staff handle more patients with less stress.
For multi-site practices, the gains are even larger. Shared scripts and templates create one voice across all locations. Patients get the same high-quality experience every time.
Curogram powers the texting and video tools that make this possible. The platform integrates with your EMR. It automates reminders. It tracks results.
Together, StreamlineMD and Curogram create a modern layer for patient communication.
The integration does not require a full overhaul. Start with one workflow. Add virtual prep for MRI. Then expand to CT, ultrasound, and IR. Each step builds momentum. Each improvement adds value.
Learn how Curogram and StreamlineMD telehealth can strengthen workflows for radiology, vascular, and IR teams. Book your demo today to see how this works for your practice.
Secure texting handles common questions like prep rules and parking. Staff manage multiple chats at once, freeing phone lines for urgent calls.
After a procedure, patients may worry about bruising or pain. A quick virtual check reassures them and lets nurses catch real problems before they get worse.
Shared templates in platforms like Curogram ensure every location sends the same instructions. This reduces confusion and builds patient trust across all sites.

💡 Telehealth helps imaging centers work faster and smarter. Virtual visits that Veradigm users rely on cut down delays and improve patient care....
💡 Telehealth in StreamlineMD helps radiology, vascular, and IR practices improve patient prep and cut day-of delays. Curogram adds HIPAA-compliant...
💡 Telehealth in Veradigm helps imaging centers handle pre-exam prep, post-visit consults, and patient coordination more easily. Fewer no-shows...