The ROI of Text-to-Pay for GE Centricity Clinics
💡 EMR-integrated payment workflows help GE Centricity clinics improve cash flow and reduce billing costs through HIPAA-compliant text payments. ...
15 min read
.jpg) Mira Gwehn Revilla
:
Updated on January 23, 2026
Mira Gwehn Revilla
:
Updated on January 23, 2026

Table of Contents
A large Oracle Health network processes thousands of patient payments each month. Every delayed payment affects cash flow. Every billing call costs staff time.
Revenue cycle efficiency for Oracle Health networks isn't just about collecting money faster. It's about building stable financial operations. Health systems need reliable cash flow to plan budgets, hire staff, and invest in patient care. When payments arrive late or require multiple follow-ups, financial planning becomes harder.
Manual billing processes create problems across the organization. Call centers spend hours reaching out to patients about unpaid bills.
Billing departments mail statements that patients ignore or forget. Staff work overtime during busy periods to keep up with payment collections. These inefficiencies add up to higher costs and lower margins.
Oracle Health networks face unique challenges at scale. Multiple facilities mean multiple billing workflows. Different departments use different collection approaches. Payment timelines vary across service lines.
Text-to-pay systems offer a solution that works across the enterprise. Patients receive payment requests by text message. They can pay from their phone in seconds.
The results are measurable. Payment timelines shrink from weeks to days. Call center volume drops as patients pay on their own.
Staff spend less time on manual follow-ups. Cash flow becomes more predictable. Financial planning improves.
For Oracle Health networks, enterprise patient communication through text-to-pay isn't just a convenience feature. It's financial infrastructure.
The right approach reduces costs, accelerates collections, and protects revenue performance while making payments easier for patients. This guide shows how health systems use text-to-pay to improve revenue cycle efficiency at every level.
Oracle Health networks process thousands of patient payments every week. Each transaction represents revenue that funds operations, pays staff, and supports patient care.
When payments arrive on time, health systems can plan confidently. When collections lag, problems spread across the organization.
Delayed collections create immediate cash flow issues. A hospital might have millions in accounts receivable but limited cash on hand.
Bills sit unpaid for 30, 60, or 90 days. During that time, the health system still needs to pay vendors, meet payroll, and cover operating costs. The gap between providing care and receiving payment strains financial resources.
Financial planning depends on predictable revenue. Budget managers need to know when money will arrive. Department heads need reliable funding for projects and staff.
Executive teams need accurate forecasts for board meetings. When payment timelines vary widely, planning becomes guesswork. Health systems lose the ability to make confident financial decisions.
Manual billing follow-ups consume valuable staff resources. Billing specialists spend hours calling patients about outstanding balances.
Call center staff field questions about confusing statements. Administrative teams process paper checks and mail reminders. This work requires trained staff, dedicated time, and ongoing attention. The cost adds up quickly across a large network.
Improving revenue cycle efficiency protects financial stability across the enterprise. Faster collections mean better cash flow. Automated processes mean lower labor costs. Predictable payment timelines mean more accurate planning.
Extended days in accounts receivable represent locked capital. Money owed sits on the books instead of in the bank. Health systems can't use those funds for operations or investments.
The longer bills remain unpaid, the harder they become to collect. Accounts aging past 90 days see collection rates drop significantly.
Increased call center volume drives up operational costs. Each outbound billing call takes staff time. Each inbound inquiry requires attention. Call centers need more staff during peak periods.
Wait times grow longer. Patient satisfaction drops. The cycle continues as more patients need help understanding their bills.
Higher operational costs reduce margins on patient care. Staff salaries, phone systems, mail costs, and administrative overhead all add to the expense of collecting payments.
For some patient encounters, collection costs can reach 10-15% of the payment amount. That overhead eats into already tight healthcare margins.
Patient frustration damages relationships and future revenue. When billing becomes stressful, patients avoid returning for care. They choose other providers. They delay needed treatments.
Poor billing experiences hurt both patient outcomes and long-term revenue. Health systems lose more than just the immediate payment.
Oracle Health networks need efficient revenue cycles to maintain financial health. The costs of inefficiency extend beyond delayed payments.
They include higher staffing needs, reduced cash flow, strained budgets, and damaged patient relationships. Addressing these challenges requires systems that work at enterprise scale across multiple facilities and departments.
Text-to-pay systems change how Oracle Health networks collect patient payments. Instead of waiting for mail or making phone calls, health systems send payment requests directly to patient phones. The process is simple, fast, and works across the entire enterprise.
Mobile payment access accelerates collections by meeting patients where they are. Most people check their phones dozens of times per day. A text message arrives instantly.
Patients see the payment request within minutes. They can complete payment in seconds without logging into portals or calling billing departments.
Automated outreach reduces delays in the collection process. Text messages go out on schedule without manual intervention.
Payment reminders arrive at optimal times. Follow-ups happen automatically. The system handles routine communication while staff focus on complex cases. This automation eliminates the lag time between services rendered and payment requests sent.
Consistent workflows improve predictability across the network. Every facility uses the same payment communication approach. Every department follows the same timeline. Every patient receives clear, standardized messages.
Faster patient response drives shorter payment cycles. When patients receive a text with a payment link, many pay immediately.
Compare this to traditional billing: mail a statement, wait for delivery, hope the patient opens it, wait for them to write a check, wait for mail return. That process takes weeks. Text-to-pay takes minutes.
Reduced reliance on mailed statements cuts both time and cost. Paper statements cost money to print and mail. They arrive days after sending. Patients misplace them or forget about them. Text messages cost pennies and arrive instantly. Patients can't lose a text in a pile of mail.
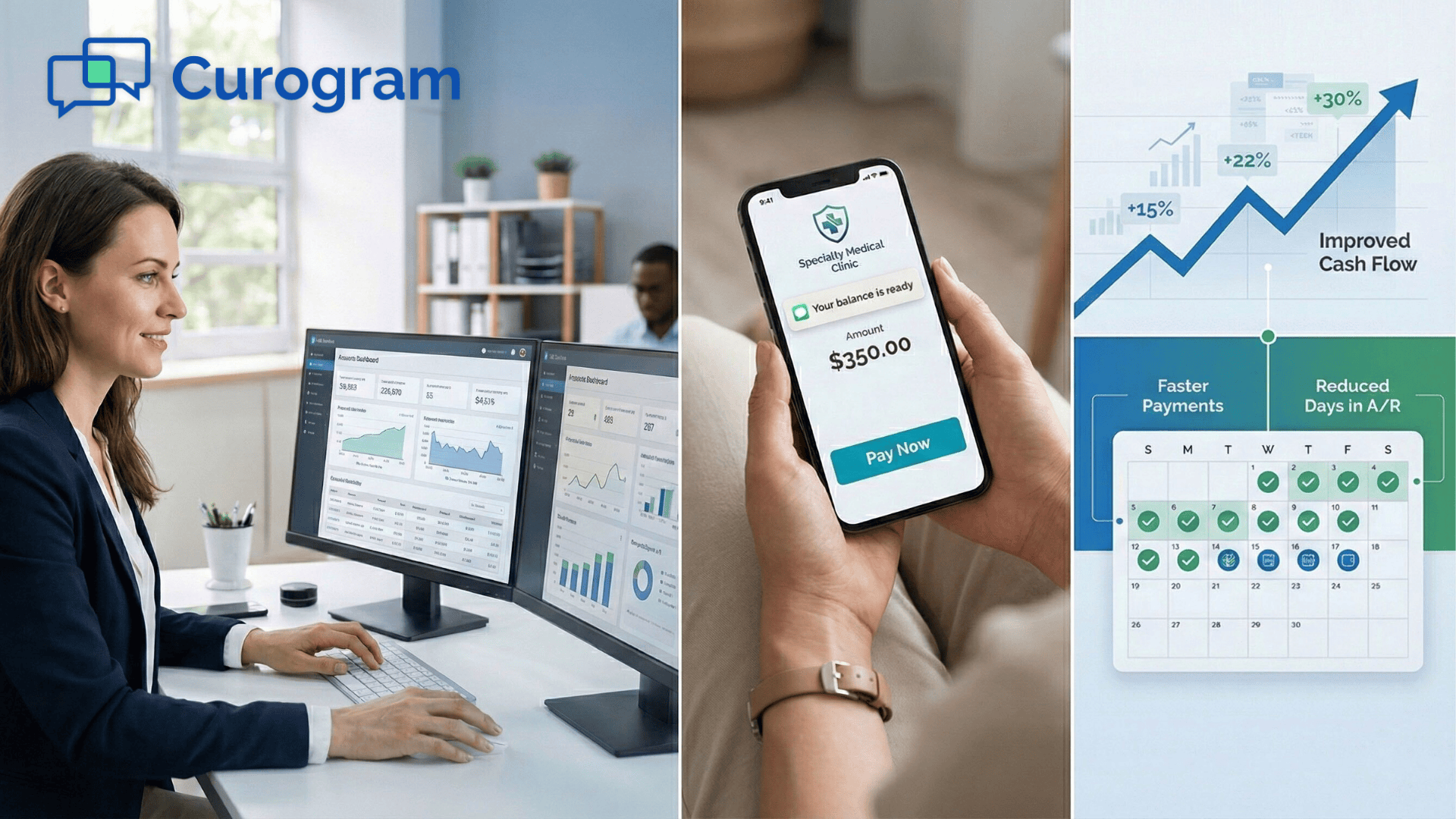
Improved cash flow results from faster payment completion. When patients pay within days instead of weeks, health systems collect revenue sooner.
Cash flow improves across the quarter. Financial managers have more working capital. Budget planning becomes more accurate. The enterprise gains financial flexibility.
A typical example:
A patient has an $800 balance after insurance. Under the old system, the hospital mails a statement. The patient receives it 5 days later. They set it aside to deal with later. Two weeks pass. The hospital sends a reminder.
Another week goes by. The patient finally calls to pay. Total time: 30 days. With text-to-pay, the patient gets a text message immediately after their visit. They click the link and pay while sitting in their car.
Total time: 15 minutes
Simple, mobile-friendly payment experiences remove barriers to payment. Patients don't need to remember passwords. They don't need to navigate complex portals. They don't need to find stamps or envelopes. They tap a link, review their balance, and submit payment.
Clear messaging improves follow-through rates. Text messages state exactly what the patient owes and why.
There's no confusion about account numbers or billing codes. Patients understand what they're paying for. Understanding leads to action.
Reduced partial or delayed payments help collections. When payment is convenient, patients pay in full. When it's complicated, they pay partial amounts or put it off entirely.
Text-to-pay reduces friction and increases full payment rates. Oracle Health networks see completion rates improve by 20-30% when payment is this accessible.
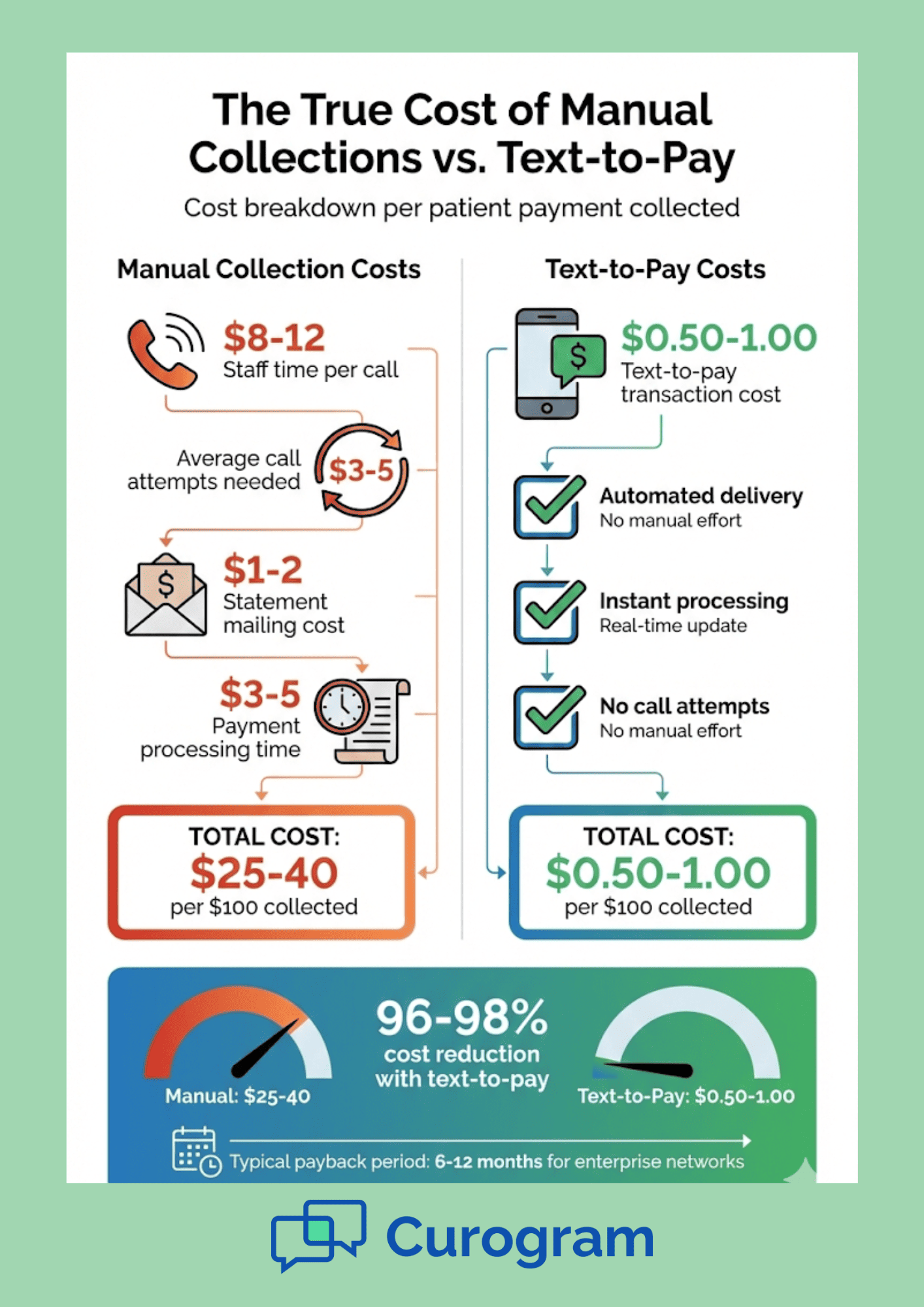
Manual collections drain resources from Oracle Health networks. Every unpaid bill requires attention. Staff make calls, send letters, and track responses.
These tasks consume time that could support patient care or other critical functions. The cost of manual collections extends beyond labor to include technology, training, and overhead.
Billing departments face constant pressure to collect more efficiently. They need to reach patients quickly, communicate clearly, and process payments accurately.
Traditional methods require significant human involvement at every step. This involvement drives up costs and limits scalability. As patient volumes grow, manual processes become unsustainable.
Automation reduces staffing pressure across billing operations. Text-to-pay systems handle routine payment communication automatically. Messages go out on schedule.
Reminders trigger based on payment status. Links remain active until payment completes. The system works 24/7 without breaks or overtime. This automation allows staff to focus on cases that truly need human attention.
Fewer outbound billing calls mean lower labor costs and better staff efficiency. Call center staff no longer spend entire days dialing patients about unpaid bills.
Automated text messages handle routine payment requests. Staff focus on patients who need assistance understanding their bills or setting up payment plans.
Reduced inbound inquiries also help call center operations. When payment communication is clear and accessible, patients have fewer questions.
They receive text messages that explain their balance clearly. They can pay without calling for help. They don't need to ask about account numbers or mailing addresses. The number of "how do I pay this bill" calls drops significantly.
Improved call center efficiency benefits patients and staff. Hold times decrease when call volume drops.
Agents handle more complex issues with greater attention. Patient satisfaction improves. Staff stress levels decrease. The call center operates more smoothly with better outcomes all around.
More predictable payment activity reduces the need for surge staffing. Traditional billing cycles create peaks and valleys in workload.
Month-end brings a surge of statements going out. Follow-up calls spike two weeks later. Staff work overtime to keep up. Then activity slows until the next cycle begins.
Text-to-pay smooths out these peaks. Payment requests go out continuously as services occur. Patients pay on rolling schedules.
The workload stays more consistent throughout the month. Billing departments don't need as many temporary staff or overtime hours to handle peak periods.
Reduced need for surge staffing improves staff morale and retention. Constant overtime leads to burnout. Unpredictable schedules make work-life balance difficult.
High turnover rates drive up hiring and training costs. More stable workloads help billing departments maintain experienced teams.More efficient operations mean better use of existing resources. These savings flow directly to the bottom line.
For example:
A billing department that regularly requires 200 hours of overtime per month to keep up with collections can eliminate most of that overtime through automation. At $35 per hour, that's $7,000 in monthly savings or $84,000 annually. Across a five-facility network, the savings multiply quickly.
The impact extends beyond direct labor costs. Supervisors spend less time managing overtime schedules. HR teams handle fewer temporary worker contracts. Payroll processing becomes simpler.
Oracle Health networks benefit from these operational improvements at scale. A text-to-pay system that works across all facilities creates consistent efficiency gains.
Central billing operations can manage higher volumes without proportional staff increases. The enterprise becomes more scalable and cost-effective.
Staff reassignment creates additional value. Hours saved on routine billing calls can support other revenue cycle functions. Staff can focus on denial management, prior authorization follow-up, or patient financial counseling.
Technology integration matters for these benefits to fully materialize. Text-to-pay systems need to work seamlessly with Oracle Health EHR systems.
Payment data needs to flow automatically into patient accounts. Billing staff need simple dashboards to monitor payment activity. When technology works smoothly, operational benefits reach their full potential.
The combination of lower call volume, reduced overtime, and better staff allocation creates a fundamentally more efficient billing operation. Oracle Health networks achieve these benefits while maintaining or improving collection rates.
Consistent collections improve financial planning across Oracle Health networks. Finance teams need reliable data to build budgets, allocate resources, and report to leadership.
When payment timelines vary widely, forecasting becomes difficult. Revenue predictions miss targets. Budget plans need constant revision. Executive teams lose confidence in financial projections.
Text-to-pay creates more predictable collection patterns. Patients receive payment requests on consistent schedules. Many pay within days. Follow-up processes happen automatically.
The variability in collection timelines decreases significantly. Finance teams can model revenue cycles with greater accuracy.
Reduced variability across departments helps enterprise-level planning. Different service lines often have different collection experiences. Emergency departments see different payment patterns than elective surgery. Primary care differs from specialty clinics. Text-to-pay standardizes the payment process across all these areas.
Faster payment cycles mean revenue arrives sooner and more predictably. Instead of waiting 45-60 days for patient payments, health systems collect within 10-15 days. This acceleration improves working capital and reduces the need for credit lines or reserves.
Better forecasting accuracy helps budget planning at all levels. Department managers know what revenue to expect. Facility leaders can plan capital projects with confidence. Network executives can commit to strategic initiatives knowing funds will arrive on schedule.
Improved financial decision-making results from better visibility. When finance teams trust their revenue forecasts, they can make faster decisions about investments, hiring, and operations. The organization becomes more agile and responsive.
Consistent workflows across service lines reduce variation in payment timing. Every department uses the same text-to-pay approach. Every patient receives the same clear communication. Every payment follows the same process.
Reduced revenue leakage protects earnings across the network. When payment processes are manual and inconsistent, some bills slip through cracks.
Patients don't receive statements. Follow-ups don't happen. Balances write off unnecessarily. Standardized automated processes catch these issues before they become losses.
Improved system-wide performance benefits the entire enterprise. When one facility improves collections through text-to-pay, best practices spread to other locations. The network learns and adapts together. Enterprise patient communication becomes a competitive advantage.
Patient satisfaction affects long-term retention and revenue. When billing experiences frustrate patients, they consider other healthcare providers.
They delay needed care. They leave negative reviews. Poor billing processes damage relationships that took years to build.
Transparent payment processes reduce friction and build trust. Patients appreciate knowing what they owe and why.e Text-to-pay delivers all these benefits while improving collection rates.
Pay from any device offers flexibility that patients value. They can pay from a phone, tablet, or computer. They can pay while sitting in their car after an appointment. They can pay during lunch breaks or evening hours.
No portal credentials required removes a common barrier. Many patients forget their portal passwords. Some never activated their accounts. Others find portals confusing to navigate. Text-to-pay bypasses all these issues with a simple link.
Clear payment context helps patients understand their bills. The text message explains what the charge is for. Patients know whether it's a copay, deductible, or balance after insurance. Understanding reduces confusion and increases payment completion.
Fewer confusing statements mean less patient anxiety about medical bills. Text messages are short and direct. They state the amount owed and provide a payment link.
Timely communication keeps patients informed throughout the payment process. They receive payment requests promptly after service.
They get reminders if payment is still pending. They receive confirmation when payment completes. This communication builds confidence and trust.

Payment communication may reference PHI that requires protection. Patient names, account balances, and service details all fall under privacy rules. Health systems must protect this information while collecting payments efficiently.
Enterprise systems require secure processes that work at scale. Oracle Health networks can't rely on individual staff members to handle every transaction securely.
They need automated systems with built-in compliance controls. Text-to-pay systems must meet these requirements to work in healthcare environments.
Secure message delivery protects patient information during payment collection. Text messages don't include sensitive details in the message body.
Payment links require authentication before displaying account information. All data transmits over encrypted connections.
Controlled access ensures only authorized users see payment details. Patients authenticate before viewing their balances. Staff access is logged and monitored. The system tracks who viewed what information and when.
Reduced compliance risk benefits the entire organization. Automated secure processes eliminate human error. Consistent workflows make audits easier. The health system demonstrates clear commitment to protecting patient privacy.
Centralized payment communication records simplify compliance reviews. All text messages are logged. Payment attempts are tracked. System access is documented. When auditors need information, it's readily available in a single system.
Clear accountability helps identify and resolve issues quickly. Each transaction has an audit trail. Staff actions are recorded. Problems can be traced to their source and corrected. This transparency supports continuous improvement.
Compliance-ready documentation protects the organization during reviews. Health systems can demonstrate they followed proper procedures.
They can show secure handling of patient information. They can prove consistent application of payment policies across the network.
Faster collections improve cash flow and working capital position. Money arrives weeks sooner. The health system can use those funds for operations instead of borrowing.
Reduced operational costs improve margins on patient care. Lower call center costs, reduced overtime, and less paper processing all contribute to better margins. These savings accumulate across thousands of transactions every month.
Fewer manual calls save direct labor costs. If text-to-pay eliminates 10,000 billing calls per month at 5 minutes per call, that's 833 hours saved. At $30 per hour including benefits, that's $25,000 in monthly savings or $300,000 annually.
Lower labor hours free staff for higher-value work. Those saved hours can support denial management, financial counseling, or other revenue cycle functions that require human expertise.
Reduced billing overhead improves department efficiency. Less printing, less postage, less payment processing time. These small savings add up across thousands of transactions to meaningful annual cost reductions.
Improved collection rates increase revenue capture. When payment is convenient, more patients pay in full. Collection rates can improve by 5-10% with effective text-to-pay implementation.
Reduced bad debt risk protects earnings. Faster collections mean fewer accounts aging past 90 days. Accounts collected early don't become bad debt write-offs. This protection is worth millions for large health systems.
Stronger financial performance supports mission and growth. Better margins fund new services, facility improvements, and technology investments. The health system can better serve its community while maintaining financial health.
Built for enterprise healthcare environments means Curogram understands the unique needs of large health systems. The platform handles high volumes, supports multiple facilities, and integrates with Oracle Health EHR systems.
Designed to support high-volume billing operations ensures reliable performance during peak periods. The system scales to handle thousands of daily payment requests without slowing down or requiring manual intervention.
Aligns payment automation with revenue operations by fitting into existing workflows. Billing teams don't need to learn entirely new processes.
Finance teams get the data they need in familiar formats. The technology enhances existing operations rather than disrupting them.
Predictable payment delivery creates consistent collection patterns across the network. Every facility benefits from the same efficient processes. Every department achieves similar performance improvements.
Centralized governance ensures consistent policies and procedures. Network administrators set payment communication standards once. All facilities follow the same approach. Compliance and quality remain high across the enterprise.
Enterprise-ready compliance meets the security and privacy requirements of large health systems. HIPAA controls are built in. Audit trails are automatic. The platform is designed for healthcare from the ground up.
Oracle Health networks need payment systems that work at enterprise scale. Text-to-pay delivers faster payments by meeting patients on their mobile devices.
Collections that once took 30-45 days now complete in days. Cash flow improves across every facility in the network.
Reduced costs come from automation that eliminates manual work. Fewer billing calls mean lower staffing needs. Less paper processing means reduced overhead. Call centers handle fewer routine inquiries.
Improved predictability helps finance teams plan with confidence. Payment timelines become consistent across departments.
Revenue forecasts gain accuracy. Budget planning relies on reliable data instead of estimates. The entire organization benefits from stable financial operations.
Text-to-pay isn't just a payment tool. It's financial infrastructure for modern healthcare networks. Like EHR systems standardized clinical documentation, payment automation standardizes revenue collection.
Oracle Health networks that invest in this infrastructure gain competitive advantages through better financial performance and improved patient experiences.
How Curogram Powers Revenue Cycle Efficiency for Oracle Health Networks
Curogram provides Oracle Health networks with a complete platform for revenue cycle efficiency through text-to-pay. The system integrates directly with Oracle Health EHR, pulling patient contact information and balance data automatically.
Billing departments don't need to export files or enter data manually. Everything flows seamlessly from the EHR to the text messaging system.
Payment requests go out based on configurable business rules. Networks can set schedules for different service lines or balance amounts. Emergency department visits might trigger immediate payment requests.
Elective procedures might wait until insurance processes. The flexibility allows each facility to optimize its approach while maintaining network-wide standards.
Patients receive clear, branded text messages that identify the health system. Messages include the payment amount and a secure link. Clicking the link takes patients to a mobile-friendly payment page. They can pay with credit cards, debit cards, or ACH transfers.
Payment confirmation arrives immediately by text. The payment posts to the patient account automatically. Billing staff see updated account balances in real time. Everything updates instantly across the system.
Analytics dashboards show payment performance across the network. Finance teams can compare facilities, service lines, or time periods. They can identify trends and optimization opportunities. Reporting tools provide the data needed for executive briefings and operational reviews.
Security features protect patient information throughout the payment process. Messages use secure delivery protocols.
Payment pages require authentication. All data transmission is encrypted. The platform maintains BAA coverage and undergoes regular security audits.
Support teams help with implementation, training, and ongoing optimization. Health systems get dedicated account managers who understand their specific needs.
Technical support is available when questions arise. The relationship continues long after initial deployment to ensure ongoing success and maximum ROI.
Revenue cycle efficiency for Oracle Health networks determines financial health across the enterprise. Faster payments mean better cash flow. Lower operational costs mean better margins. More predictable collections mean more confident planning.
Text-to-pay transforms patient payment collection from a manual, costly process into an automated, efficient system. Patients get convenient payment options that fit their preferences. Health systems get faster revenue collection with less staff effort. Both sides benefit from the improved approach.
The financial impact extends beyond direct collection improvements. Call centers operate more efficiently.
Billing departments handle higher volumes without adding staff. Finance teams make better decisions with more accurate forecasts. The benefits ripple through the entire organization.
Patient relationships improve when billing processes become simple and transparent. Convenient payment options reduce frustration. Clear communication builds trust. Positive billing experiences support long-term patient retention and loyalty.
Compliance protection comes built into automated payment workflows. Secure messaging protects patient privacy. Audit trails support regulatory requirements. Enterprise systems maintain consistent standards across all facilities.
Oracle Health networks face unique challenges at scale. Multiple facilities, diverse patient populations, and complex billing scenarios all require sophisticated solutions. Text-to-pay systems designed for enterprise healthcare meet these needs while delivering measurable ROI.
The path forward is clear. Health systems that automate patient payment collection gain competitive advantages. They collect revenue faster, operate more efficiently, and serve patients better. Enterprise patient communication through text-to-pay isn't optional for networks focused on financial performance.
Curogram helps Oracle Health networks achieve these benefits through purpose-built technology and dedicated support. The platform delivers revenue cycle efficiency improvements while maintaining the security and compliance standards healthcare requires.
Book a demo to see how Curogram supports better care workflows with Oracle Health.
Discover purpose-built technology and dedicated support. Book a demo today to see how Curogram delivers revenue cycle efficiency while maintaining security and compliance.
Calculate cost savings from reduced call center hours, lower overtime, and decreased mail expenses. Factor in revenue improvements from faster collections and higher payment rates. Most Oracle Health networks see ROI within 6-12 months through combined operational savings and accelerated cash flow.
HIPAA-compliant text-to-pay systems use secure message delivery, encrypt data transmission, and require authentication before showing account details. Messages don't include sensitive information in the text body. All access is logged and monitored to meet healthcare privacy standards.
Text-to-pay automation reduces routine outbound call volume by 30-40%, allowing existing staff to focus on complex accounts requiring personal attention. Health systems typically maintain staff levels while handling higher patient volumes, or reallocate hours to other revenue cycle functions.
💡 EMR-integrated payment workflows help GE Centricity clinics improve cash flow and reduce billing costs through HIPAA-compliant text payments. ...
💡 Text-to-pay helps imaging centers improve cash flow with Veradigm by speeding up payment collection. It cuts down the time patients take to pay...
💡 Text-to-pay for Oracle Health systems helps large healthcare networks collect patient payments faster and reduce billing workload. This approach...