Delivering Radiology Virtual Consults with Telehealth in Ramsoft
💡 V irtual visits in Ramsoft help you connect with patients who need crucial follow-ups. People struggle to return in person because of distance,...
10 min read
Aubreigh Lee Daculug
:
January 28, 2026
Table of Contents
Imagine a patient who just completed a complex cardiac MRI at your imaging center. They’re anxious, replaying the exam in their head, and eager for answers. They need to speak with their cardiologist—but coordinating that follow-up quickly turns into a logistical maze.
Your front desk team starts making phone calls. Voicemails stack up. The patient struggles to find time off work. Meanwhile, the radiologist’s findings sit in the queue, waiting for review. Multiply this by dozens of patients each week, and the inefficiencies become impossible to ignore.
Medstreaming locations manage thousands of scans every year. Each exam triggers a critical chain of communication—results delivery, provider review, patient questions, and follow-up care. Yet many centers still rely on workflows built for a different era: in-person visits, manual scheduling, or generic telehealth apps patients never download.
The outcome is predictable. Follow-ups are delayed. Patients feel left in the dark. Staff are stretched thin, spending valuable hours coordinating care instead of supporting throughput and growth.
Virtual visits within Medstreaming environments should be effortless for both patients and providers. Patients expect quick access to results without downloading apps, creating accounts, or navigating unfamiliar technology. Providers need efficient consultations without adding new systems or workflows.
HIPAA-compliant telehealth delivers this only when it’s built for imaging operations. Generic video platforms don’t support radiology or cardiovascular workflows, lack Medstreaming integration, and add administrative friction—pushing coordination back onto your staff.
Now imagine a different experience.
A patient receives a text message. They tap once and instantly join a secure virtual consultation. No app downloads. No passwords. No technical barriers. Just direct access to their provider at the moment it matters most.
This is the standard modern imaging centers are setting today. By removing friction and automating communication, they’re redefining how follow-up care is delivered. Remote consultations become effortless. Results are reviewed faster. Patients stay engaged. Staff regain time and control.
The technology to make telehealth seamless in radiology and cardiovascular imaging already exists. The real question is no longer if imaging centers should adopt it—but how to implement telehealth in a way that truly supports Medstreaming workflows, patient expectations, and operational performance.
Walk into any busy imaging center on a Tuesday morning and the pattern is familiar. Phones ringing nonstop. Front desk staff juggling calls while patients wait for results. Voicemails stack up faster than anyone can return them. Even well-run teams feel the strain.
Every CT, MRI, echo, and vascular study triggers follow-up. Results need review. Patients want answers—quickly. Demand for post-scan consultations keeps rising, pushing traditional workflows to the edge.
The phone quickly becomes the biggest bottleneck. Staff spend hours calling patients, often reaching voicemail again and again. When callbacks finally come in, they hit during peak hours, driving longer hold times and mounting frustration on both sides.
In-person follow-ups don’t solve the problem. No-show rates climb because the scan already felt like “the visit,” or patients can’t take more time off work. Others face long drives for what they expect will be a short conversation.
And they’re right. Many of these appointments last ten minutes. Images are reviewed. Findings explained. Questions answered. Physical exams are rarely needed—yet patients lose hours to travel and waiting.
App-based telehealth promised relief, but introduced new friction. Long emails, download links, account creation, and setup steps stopped many patients before they ever joined a visit. Older cardiovascular patients struggled most, and support calls flooded front desk lines instead.
Staff spent hours answering questions that had nothing to do with patient care:
“The app won’t download on my phone.”
“My password doesn’t work.”
“The camera is just a black screen.”
“Which app am I supposed to use?”
Multi-location imaging centers faced a bigger problem. Different sites used different telehealth platforms, forcing patients to juggle multiple apps and logins from visit to visit.
Staff training became confusing and inconsistent. New hires learned several systems, while experienced teams double-checked platforms before every appointment. Even sending a telehealth link depended on the location and provider.
Manual coordination only added strain. Follow-ups, links, messages, and reminders were handled one by one. At scale, burnout was inevitable.
Errors piled up. Links went to the wrong patients. Appointments landed on the wrong platform. Some patients never received access at all, while timing pressures increased daily stress.
This wasn’t better care—it was operational chaos. Staff worked harder, patients grew frustrated, and providers lost time troubleshooting technology instead of reviewing scans.
Imaging centers didn’t need another tool. They needed a solution designed around how radiology and cardiovascular teams actually work—simple, unified, and built for daily operations.
Here’s the core issue: traditional telehealth platforms were built for primary care seeing 20 patients a day—not imaging centers managing 200 follow-ups a week. That mismatch creates friction at scale. What works for a small clinic breaks under imaging volume.
App downloads are the first barrier. Most platforms require patients to install software, create accounts, and manage passwords. In theory, that’s fine. In practice, it stops patients before care even begins—especially older adults.
Consider Maria, a 68-year-old cardiac MRI patient. She’s already anxious about her results. Now she’s navigating app stores, setup emails, and account creation. Instead of reassurance, the process adds stress.
Those steps trigger a flood of support calls. Patients can’t find the right app. Password emails get lost. Some apps won’t install at all. Front desks become tech support.
Multiple platforms make it worse. Imaging networks often inherit different systems at different locations. Patients download one app for one site, another app for the next. Confusion becomes routine.
Staff training suffers. New hires learn multiple systems. Experienced teams rely on reminders and workarounds. Even sending a telehealth link depends on location and provider.
Manual coordination drains time when the telemedicine workflow isn’t automated. Staff manually generate remote consultation links, copy and paste messages, and repeat the process dozens of times a day—each step increasing the risk of errors.
Integration gaps force constant workarounds. Imaging schedules live in one system. Telehealth lives in another. Staff manually connect them, appointment by appointment.
Automation is absent. Every follow-up requires human effort—scheduling, links, messages, reminders. Scale that weekly and inefficiency is inevitable.
Security adds another layer. Each platform brings different HIPAA reviews, training requirements, and documentation standards—raising risk with every added system.
The result is cumulative drag. What should take seconds takes minutes. Patients grow frustrated. Staff burn out. Providers lose focus.
This isn’t telehealth’s promise. It’s what happens when tools built for primary care are forced into imaging environments. Imaging centers don’t need retrofits—they need solutions designed for how they actually operate.
Imagine telehealth that works like texting—because that’s exactly what it is. No-app telehealth replaces complexity with a single text message and a secure link that opens the visit instantly in the patient’s browser. No downloads. No accounts. No setup.
Patients simply tap the link and connect face-to-face with their provider. It works on any smartphone using the browser already on the device, removing the barriers that stop traditional telehealth before it starts.
The experience shifts from frustrating to effortless. A reminder arrives—“Your imaging follow-up is in 30 minutes. Tap to join.” One tap starts the visit using tools patients already know.
For imaging centers, the payoff is immediate. App-related support calls disappear. Staff stop troubleshooting technology and return their focus to patient care.
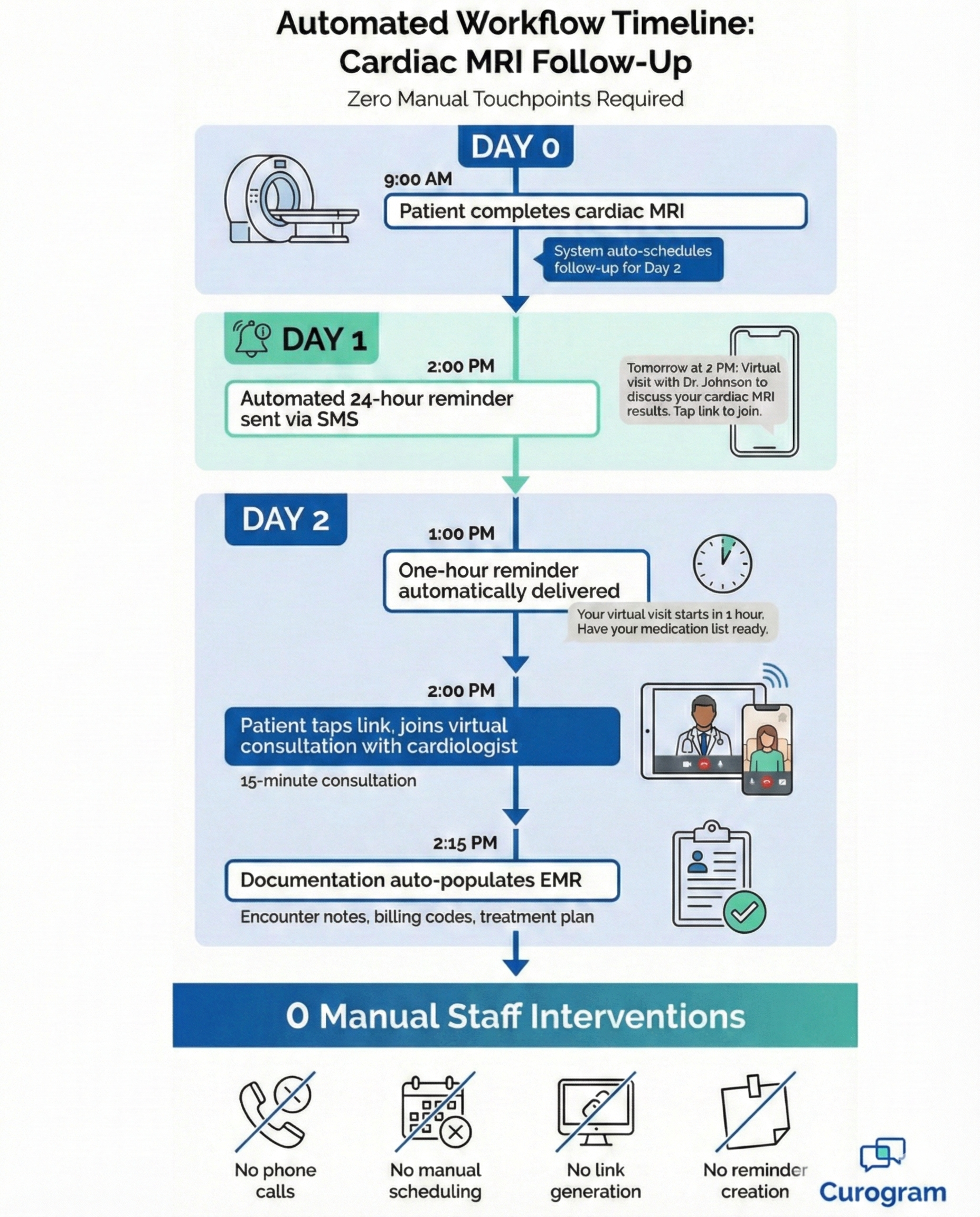
Automation handles the rest. Follow-up visits schedule automatically based on scan type and result timing. Pre-scan and post-scan workflows run in the background without manual coordination.
Smart routing ensures patients connect with the right provider every time—based on modality, specialty, and provider preferences—without staff managing complex rules.
This is telehealth built for imaging: simple for patients, efficient for staff, and aligned with how imaging centers actually operate.
Multi-location imaging centers gain seamless coordination. Patients can scan at one location and consult with their preferred cardiologist at another—without confusion or manual effort. The system handles routing automatically.
Adoption is instant across all demographics. There’s nothing new to learn—patients receive a text, tap a link, and join. Familiar behaviors replace onboarding friction.
This simplicity is especially effective for older cardiovascular patients. Text-based access feels natural, not intimidating, making virtual visits easier to accept and complete.
Security stays invisible. Links are encrypted, time-limited, and HIPAA-compliant. No sensitive data is sent by text—only secure access.
Staff training drops from days to minutes. One system serves every provider and location, eliminating platform confusion and preference tracking.
Deep integration keeps workflows moving. When scans are marked complete in RIS, follow-up visits schedule automatically. PACS ensures images are ready for review. No manual handoffs required.
Urgent findings move fast. Stat reads trigger immediate telehealth access, while routine screenings follow standardized timelines.
Patients arrive prepared. Automated messages share clear expectations and prompts before visits, leading to more productive conversations.
Smart reminders reduce no-shows. Evidence-based timing sends 24-hour and 1-hour alerts, with simple text replies to reschedule if needed.
Provider schedules stay aligned. Telehealth availability mirrors blocked review times, prevents double-booking, and adjusts visit lengths based on exam complexity.
Documentation flows directly into the medical record. Virtual visit notes populate patient charts instantly, supporting compliance and billing without extra effort.
Scalability is built in. The same workflow supports 50 scans a day or 500—without added staff or complexity.
Analytics reveal what’s working and where to improve, from provider adoption to follow-up performance.
ROI shows up fast. Call volume drops, compliance improves, and centers grow without rising costs.
The integration between Medstreaming imaging centers and Curogram's telehealth platform creates seamless workflows designed specifically for radiology and cardiovascular imaging. This synchronization addresses the unique needs of high-volume imaging environments while maintaining simplicity for patients and staff.
Pre-scan virtual assessments prepare patients before complex imaging exams. Cardiologists review history, symptoms, and medications in short video visits to catch issues early.
Links send automatically based on exam type—advanced procedures require assessments, routine screenings don’t.
This reduces day-of cancellations and ensures patients arrive properly prepared.
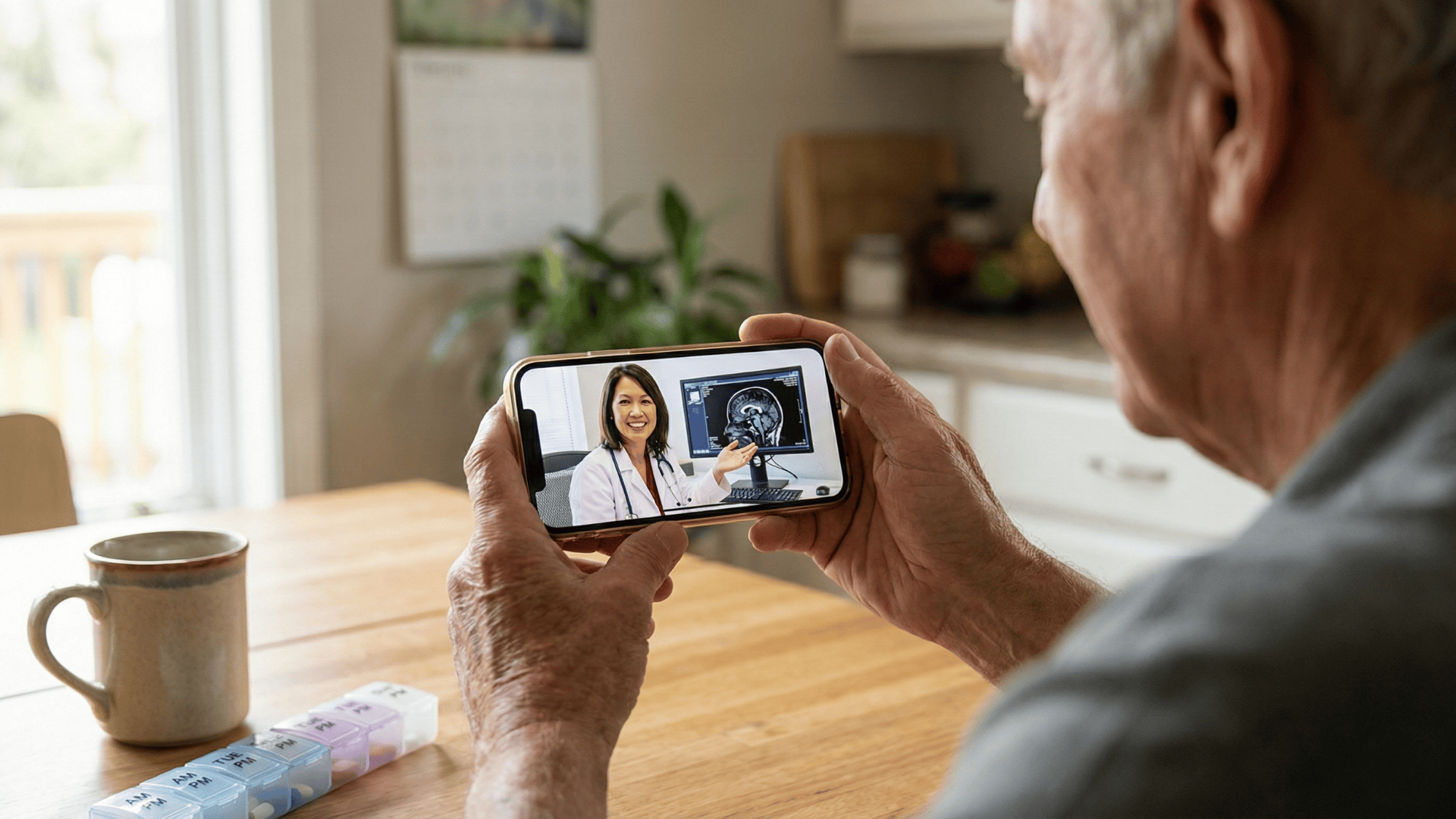
Results review is one of the highest-value telehealth use cases in imaging. Patients get timely discussions of findings without unnecessary in-person visits, reducing anxiety and speeding treatment decisions.
Reviews schedule automatically based on exam type and read time—routine studies follow standard timelines, while urgent findings trigger same-day consults.
During visits, providers share imaging on screen, making virtual results reviews as effective as in-person discussions.
Automation removes the manual work that once burdened front desk teams. After a scan is completed, the system drives the telemedicine workflow by determining the required follow-up, scheduling the virtual visit, sending the access link, and updating the provider’s calendar automatically.
Staff step in only when exceptions arise, reducing administrative load while improving follow-up consistency.
The impact on staff workload is transformative. Tasks that once required calls, emails, and manual scheduling now run automatically, freeing staff to focus on patient education and care coordination.
Front desk phone volume drops as patients receive clear, automatic visit links by text—eliminating most follow-up questions.
Different imaging modalities benefit from telehealth in unique ways. Understanding these specific applications helps imaging centers maximize virtual care value.
Cross-sectional imaging often reveals incidental findings that need discussion, not an in-person visit. Virtual consultations let radiologists explain results, recommend next steps, and coordinate referrals—saving patients unnecessary trips.
Serial imaging for chronic conditions benefits from consistent virtual follow-ups. Patients with heart failure receiving regular echocardiograms can review trends with their cardiologist remotely. This continuity supports better disease management without increasing travel burden.
Cardiac and vascular studies frequently need cardiologist interpretation beyond the written report. Virtual visits enable providers to review moving images with patients, explaining valve function or blood flow patterns. This visual review builds patient understanding and supports treatment decisions.
Post-operative imaging requires clear explanation of healing progress. Surgeons can review imaging virtually with patients, explaining what they see and what it means for recovery. This reassures patients and provides clear next-step instructions without requiring office visits.
Procedures requiring significant preparation benefit from virtual education sessions. Patients can ask questions about fasting requirements, medication adjustments, or what to expect during the scan. This reduces anxiety and improves compliance with preparation instructions.
No-app telehealth and telemedicine platforms like Curogram deliver measurable efficiency gains across imaging center operations. These improvements compound over time as staff rely more on automation and patients adopt simpler, text-based workflows.
Reducing unnecessary in-person visits frees appointment slots for patients who truly need on-site care. Imaging centers increase capacity without expanding physical space or extending hours—an important financial advantage given the cost of medical facilities.
Call volume drops almost immediately. Automated scheduling and clear visit links reduce outbound coordination calls, while inbound questions decline as patients receive timely, intuitive communication.
Faster results reviews benefit both patients and providers. Discussions happen in days instead of weeks, reducing patient anxiety and allowing treatment decisions to move forward sooner when action is needed.
Patient satisfaction improves as convenience and communication increase. These gains influence online reviews and provider choice, directly impacting referral volume.
Operational data reinforces the value. Centers handle significantly more follow-up consultations with the same staff, virtual visit no-shows fall well below in-person rates, and staff burnout decreases as workflows stabilize.
Together, these efficiency gains create a competitive advantage—helping imaging centers attract patients, retain staff, and grow revenue without adding complexity.
Imaging centers can’t afford outdated communication workflows. Scan volumes continue to rise while patient expectations for convenience grow. Traditional follow-up processes create bottlenecks that slow care and frustrate patients, providers, and staff alike.
No-app telehealth removes these barriers while improving the patient experience. Medstreaming locations using SMS-based virtual visits see fewer phone calls, higher follow-up compliance, and stronger patient satisfaction. Staff report less stress and more efficient daily workflows.
The technology is available today—and it doesn’t require large IT projects or long training cycles. SMS-delivered virtual visits are intuitive, enabling fast adoption across teams and patient populations.
Starting with high-impact use cases like results reviews builds early momentum. Providers see immediate value, staff gain confidence, and positive patient experiences reinforce adoption.
The return is immediate. Reduced call volume saves staff time, improved follow-up supports better outcomes, and automation allows centers to grow without rising costs.
For Medstreaming imaging centers ready to modernize follow-up care, Curogram delivers a purpose-built solution designed specifically for imaging workflows and patient communication needs.
Book your demo now and discover how automated workflows, SMS-delivered virtual visits, and seamless integration can transform your imaging center's telehealth capabilities.
Patients receive a simple text message with a secure link. Tapping it opens the video visit in their phone’s web browser—no apps, accounts, or passwords required. If a patient can read a text, they can join a visit, making it accessible even for older adults.
Imaging centers require automation, image screen-sharing, and tight integration with radiology systems. Generic platforms rely on manual scheduling and don’t support high-volume, time-sensitive follow-ups. Imaging-specific solutions are built to handle these workflows efficiently.
The system uses rules based on exam type, read times, and provider preferences. Urgent findings trigger rapid follow-ups, while routine studies schedule later. Provider availability is factored in automatically, eliminating manual coordination.
Imaging results contain highly sensitive patient data. HIPAA-compliant platforms use encrypted connections and secure links, never sending clinical information via text. Compliance protects patient privacy and reduces legal risk.
Virtual visits are just as effective for most results reviews. Providers can share images on screen, and patients benefit from convenience and faster access—often improving follow-up compliance. In-person visits are scheduled only when physical exams are needed.
💡 V irtual visits in Ramsoft help you connect with patients who need crucial follow-ups. People struggle to return in person because of distance,...

💡 Virtual visits in Exa allow secure communication with patients at your convenience. When follow-ups happen only in person, many people skip...
💡 Telehealth in Veradigm helps imaging centers handle pre-exam prep, post-visit consults, and patient coordination more easily. Fewer no-shows...