Professional Text Communication in Healthcare: A Complete Guide
💡 Professional text communication in healthcare refers to the use of secure, HIPAA-compliant patient texting to manage appointments, share...

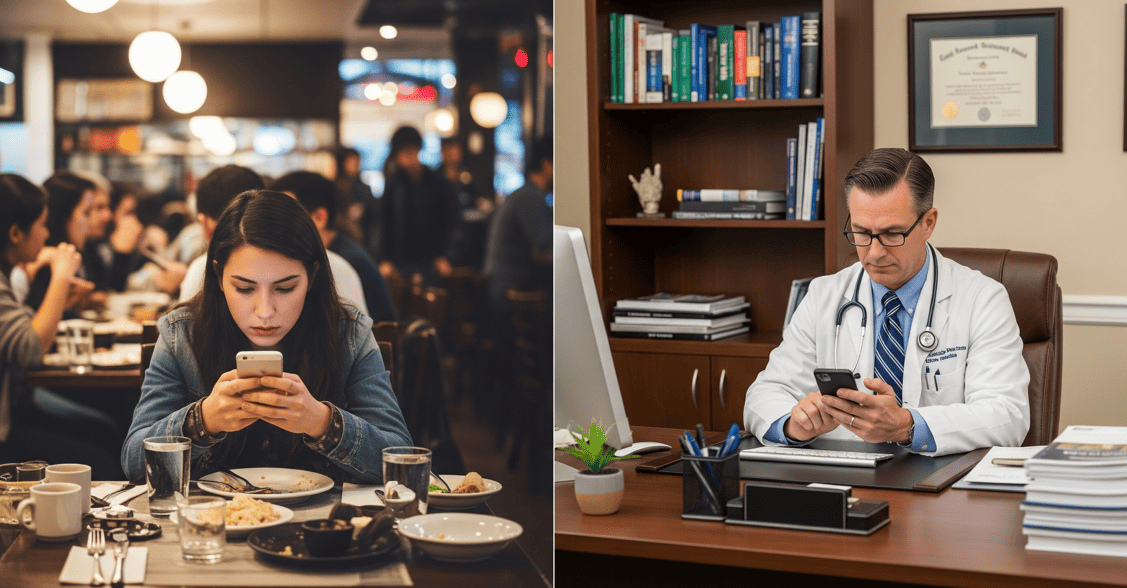
A patient sends an angry text at 3 p.m. on a busy Monday. The front desk is slammed. The phone rings nonstop. And now, those sharp words on the screen demand a quick, careful reply.
This scene plays out every day in medical offices across the country. Text messaging has become a core tool for patient outreach. But it also opens the door to conflict. When a patient is upset, a text thread can spiral fast.
The problem is clear. Text strips away vocal tone and facial cues. A short reply meant to be helpful can read as cold or rude. Patients may type things they would never say face-to-face. Delayed responses can make frustration grow.
Managing patient complaints via text is now a must-have skill for every front desk team. Without the right words, a small issue can become a formal complaint or a lost patient. With the right approach, that same tough exchange can build deeper trust.
This guide gives you a proven system for handling these moments. You will learn a five-step framework for any difficult patient communication. You will find over 30 ready-to-use scripts for billing issues, scheduling conflicts, and care concerns. You will also learn when to move the conversation off text and onto a call.
Whether you deal with an angry patient text response once a week or ten times a day, these tools will help. The goal is not to avoid hard conversations. It is to handle them in a way that protects both your patients and your team. For broader tips on messaging best practices, see our guide to professional text communication in healthcare.
Text-based conflict is not the same as a phone call or in-person exchange. The rules shift when you cannot hear a voice or see a face. Knowing these differences helps your team prepare.
The biggest factor is the lack of vocal tone and body language. In a phone call, a warm voice can calm a nervous patient in seconds. Over text, that same warmth has to come through words alone. A message like "We can help" may read as sincere to one person and dismissive to another.
Delayed response time also plays a role. When a patient fires off a frustrated message, every minute of silence feels longer. A ten-minute gap that seems short to your busy staff can feel like being ignored to a patient who is upset. This gap can increase anger before a reply ever goes out.
The written record cuts both ways. Every message is saved. This is useful for tracking issues and staying compliant. But it also means a careless word lives on. Patients can reread a reply, focus on one phrase, and feel worse over time.
Patients also tend to be more direct over text. The distance of a screen can make people bolder. They may use harsh language or make demands they would soften in person. This is part of why challenging patient conversations feel tougher in a text thread.
There is a bright side, though. Text gives you time to think. You can draft, review, and polish a reply before you send it. You can loop in a colleague. You can pick the right words for a tricky situation. When used well, this pause can help you de-escalate patient anger text message exchanges before they get worse.

A strong framework takes the guesswork out of crisis moments. When your staff knows exactly what to do, they respond with confidence instead of panic. This five-step system works for nearly every type of difficult exchange over text, from billing disputes to care concerns.
The urge to reply right away is strong. An angry message sits on the screen, and every instinct says to answer fast. But quick replies to heated messages almost always make things worse. The first step in any tough text exchange is to stop and breathe.
Use what we call the five-minute rule. When a message carries strong emotion, wait at least five minutes before you type. This short pause helps you shift from reactive to thoughtful. It also lowers the chance of sending something you will regret.
During that pause, check your own state. Are you stressed from a long day? Are you taking the words personally? If so, you are more likely to fire back with a sharp reply. Read the message at least twice. Often, the second read reveals context you missed the first time.
For very heated messages, loop in a colleague or supervisor. A second set of eyes can spot tone issues in your draft and suggest a better angle. This review step is a key part of any conflict resolution texting healthcare teams can adopt.
Once you are calm and ready, the next move is to show the patient you hear them. This does not mean you agree with every claim. It means you respect their feelings. People calm down faster when they feel seen.
Start your reply with a line that names their emotion. Phrases like "I can see this has been frustrating for you" or "I understand this is not the experience you expected" go a long way. This is the heart of patient de-escalation techniques that work in text.
Avoid any language that sounds defensive. "Well, actually..." or "That's not what happened" will pour fuel on the fire. Even if the patient has the facts wrong, your first job is to connect, not to correct.
The "feel, felt, found" method works well here. You might say: "I understand how you feel. Others have felt the same way in this situation. What we have found is that we can usually resolve this quickly." This shows empathy in crisis situations without admitting fault.
Here are some validation phrases your team can use right away:
Template 1: "I hear you, and I want to make this right."
Template 2: "Thank you for letting us know. Your concerns matter to us."
Template 3: "I understand this is stressful. Let me look into this for you."
Template 4: "I can see why this would be upsetting. Let us help."
Template 5: "You deserve a better experience, and I want to fix this."
Template 6: "I appreciate you reaching out. We take this seriously."
Template 7: "That sounds really frustrating. I am going to find answers for you."
For a deeper look at expressing empathy over text, see our comprehensive guide on 40+ powerful ways to express empathy over text.
After you validate, decide if an apology fits. Not every situation calls for one. But when your practice dropped the ball, owning it builds trust fast. Patients can sense a hollow apology, so keep it real.
A good apology is specific. "I'm sorry for the wait" is better than a generic "I'm sorry." Tell the patient what went wrong, at least in broad terms. For example: "I'm sorry your call was not returned yesterday. That is not our standard, and I can see why you are upset."
Be careful about what you claim fault for. In healthcare, there are legal lines you should not cross. Do not admit to clinical errors over text. If the issue involves a medical concern, it is best to move to a phone call or in-person meeting. Stick to service-level apologies in text threads.
Avoid over-apologizing, too. Saying sorry five times in one message can sound insincere or anxious. One clear, direct apology paired with a plan of action is far more effective.
Try these apology templates:
Template 1: "I am sorry this happened. Here is what we are doing to fix it."
Template 2: "You are right, and I apologize. We should have handled this better."
Template 3: "I'm sorry for the confusion. Let me clear this up for you now."
Template 4: "This was our mistake, and I take full ownership. Let me make it right."
Empathy without action falls flat. After you acknowledge and apologize, give the patient a clear next step. Vague promises like "We'll look into it" leave patients feeling brushed off. Specific plans build confidence.
Tell the patient exactly what will happen and when. Include a timeline. "I am going to review your account and call you by 3 p.m. today" is far stronger than "I'll get back to you soon." This level of detail shows you take their concern seriously.
Some issues need a team effort. If the right person to help is a billing specialist or a nurse, say so. Let the patient know who will follow up and how. This step is central to effective patient conflict management messaging.
Certain conversations should move off text. If the issue is complex, emotional, or involves clinical details, offer a phone call. This is not a retreat. It is a smart move that protects both the patient and the practice.
Here are solution templates you can adapt:
Template 1: "Here is what I am going to do. I will review your chart and have our team leader call you by end of day."
Template 2: "I want to make sure we fix this. Can I have our billing team reach out to you within the hour?"
Template 3: "Let me connect you with the right person. Our scheduling lead will text you in the next 30 minutes."
Template 4: "This deserves a full conversation. Would you be open to a quick phone call so we can sort this out together?"
Template 5: "I have flagged this for our office manager. You will hear from them by tomorrow at 10 a.m."
Template 6: "We want to get this resolved today. I am pulling your records now and will follow up within two hours."
Template 7: "Thank you for your patience. I have scheduled a callback for you at 4 p.m. today with our care team."
The final step is often the one teams skip. Following up after a tough exchange is what separates good service from great service. It shows the patient that their concern was not forgotten.
Start by logging the issue. Document what happened, what was said, and what was promised. This record helps if the issue comes up again. It also protects your practice from a compliance standpoint.
Set a reminder to check in. Even a simple text like "Hi, I wanted to follow up and make sure everything was resolved" can make a lasting impression. This closing step is a core part of healthcare customer service texting.
After the issue is closed, debrief with your team. What went well? What could improve? Every hard conversation is a chance to learn. Over time, these reviews sharpen your staff's skills and build a stronger response culture.
Use these follow-up messages:
Template 1: "Hi, I wanted to check in. Were you able to get everything sorted out? Let us know if you need anything else."
Template 2: "Just following up on our conversation from Tuesday. I hope things are going well. We are here if you have questions."
Template 3: "We value your feedback. Is there anything else we can do to make your experience better?"
Ready-made scripts take pressure off your staff in the heat of a tough moment. Adapt these to fit your practice's voice, but keep the core of each message: empathy, clarity, and a path forward. These difficult conversation scripts cover the most common scenarios your team will face.
Billing issues rank among the top reasons patients get upset. Confusion over charges, surprise bills, and denied claims can trigger strong reactions. Complaint handling healthcare teams know that money is personal. A calm, clear response makes all the difference.
Patient: "I just got a bill for $400. Nobody told me I would have to pay this. This is ridiculous."
Response: "I understand this is frustrating, and I want to help. Let me pull up your account and review the charges. I will text you back within 30 minutes with a clear breakdown."
Patient: "My insurance was supposed to cover this. Why am I getting a bill?"
Response: "I hear you. Insurance billing can be confusing. Let me check with our billing team to see what happened. I will have an answer for you by the end of today."
Patient: "I can't afford to pay this all at once. What are my options?"
Response: "Thank you for reaching out. We have payment plan options that may help. I will have our billing coordinator contact you today to walk through the details."
Patient: "I keep getting bills for something that should be covered. I have called three times and nothing changes."
Response: "I am sorry you have had to follow up so many times. That is not acceptable, and I want to fix this now. I am escalating your case to our billing supervisor. You will hear from them by tomorrow at noon."
Scheduling problems are another big source of patient frustration. Long waits, last-minute changes, and trouble getting an appointment all test patience. When you need to handle upset patients text exchanges about scheduling, speed and a clear fix are everything.
Patient: "I have been waiting for 45 minutes past my appointment time. This is so disrespectful."
Response: "You are absolutely right to be frustrated, and I sincerely apologize for the delay. The provider is running behind due to an urgent situation. I want to make this right. Would you like to wait, or can I reschedule you at a priority time slot?"
Patient: "You changed my appointment without even asking me. I took the day off for this."
Response: "I am so sorry about this. Changing your appointment without checking with you first was wrong. Let me find a time that works for your schedule right away."
Patient: "I have been trying to get an appointment for two weeks. Nobody calls me back."
Response: "I am sorry for the delay and the missed calls. You should not have to chase us down. I am checking our schedule right now. Can I book you in for the next available slot?"
Patient: "I showed up and was told my appointment is not until next week. I have the confirmation text right here."
Response: "I can see how confusing and frustrating that must be. Let me review our records right now. If we made the error, I will get you seen today or at the soonest available time."
When a patient has concerns about their care, the stakes go up. These conversations require extra thought. Some should be handled by phone or in person, not over text. Always consider whether a clinical topic is safe for text before you reply.
Patient: "I don't agree with my diagnosis. I feel like the doctor didn't listen to me at all."
Response: "I hear your concern, and I want you to feel confident in your care. This kind of conversation is best over the phone. Can I have your provider's team call you today to discuss this further?"
Patient: "This medication is giving me terrible side effects. I want to stop taking it."
Response: "I am sorry you are dealing with that. Please do not stop the medication before speaking with your provider. I am sending a message to them right now, and they will reach out to you today."
Patient: "I feel like my symptoms were brushed off. I expected better care."
Response: "Your health concerns matter to us, and I am sorry you felt that way. I would like to arrange a follow-up so your provider can give you more time. Would a callback or a new appointment work better?"
Patient: "I want a second opinion. How do I go about that?"
Response: "That is completely your right, and we support you. I will have our referral coordinator reach out to help set that up. Expect a call or text within one business day."
Important note: If a patient describes urgent symptoms or a potential emergency, stop texting immediately. Direct them to call 911 or go to their nearest emergency room. Never attempt to manage a crisis communication text messaging thread when safety is at risk.
Patients expect to be heard. When calls go unreturned or messages sit without replies, trust erodes. These scripts help repair that trust. Timely patient dissatisfaction management starts with owning the gap.
Patient: "Nobody ever returns my calls. I have left three messages this week."
Response: "You are right, and I am sorry. Three unreturned calls is not okay. I am personally looking into this now and will make sure someone gets back to you within the hour."
Patient: "Your receptionist was rude to me on the phone."
Response: "I am sorry to hear that. You deserve to be treated with respect every time you contact us. I am sharing your feedback with our office manager so we can address this."
Patient: "I have been waiting for my test results for two weeks. Can someone please update me?"
Response: "I understand the wait must be stressful. Let me check on the status of your results right now. I will text you back within the next hour with an update."
Patient: "I was told I would get a referral last week. Nothing has come through."
Response: "I apologize for the delay. I am following up with our referral team right now. I will make sure you have an update by end of day today."
Office policies exist for good reasons, but patients do not always see it that way. When someone pushes back on a rule, the key is to explain the "why" with empathy. Firm does not have to mean cold.
Patient: "Why do I have to fill out all this paperwork again? I was just here last month."
Response: "I know it feels like a lot. We update records regularly to make sure your care is accurate and up to date. I appreciate your patience with this. It only takes a few minutes and helps us serve you better."
Patient: "I can't believe you charged me a cancellation fee. I had an emergency."
Response: "I am sorry about the charge, and I understand emergencies happen. Let me review your account. If this was your first cancellation, we may be able to waive the fee."
Patient: "Why do I have to pay before I see the doctor? That seems unfair."
Response: "I understand your concern. Collecting copays before the visit is our standard process to keep billing simple for everyone. If you have questions about your balance, I can connect you with our billing team."
Patient: "Your insurance verification process is way too slow. I almost missed my appointment."
Response: "I am sorry about the delay. We check insurance to avoid surprise charges for you. I will look into why it took so long and make sure it does not happen again."
Not every conversation belongs in a text thread. Some situations need a live voice, a face-to-face meeting, or even emergency services. Recognizing these red flags fast can prevent harm and protect your practice.
Move off text right away if a patient signals a medical crisis or emergency. If someone describes chest pain, severe bleeding, or thoughts of self-harm, direct them to call 911 or their nearest ER. Never try to manage urgent medical needs through text.
Threats of violence also require an immediate channel switch. If a patient uses language that threatens staff or themselves, document the message and involve your supervisor. This is not a text conversation. It needs direct human contact and, in some cases, local authorities.
Watch for anger that keeps rising despite your best efforts. If you have tried to validate, apologize, and offer solutions but the patient is still escalating, a phone call is the better path. Patient service recovery works best when the patient can hear your tone and feel your care.
Complex medical discussions should also move off text. A treatment plan change, a difficult diagnosis, or a detailed care conversation needs the richness of voice. Text is great for logistics. It is not ideal for clinical depth.
If legal or liability concerns come up, switch channels. The same goes for potential HIPAA issues. If a patient shares protected health information in a non-secure text, address it quickly by moving to a compliant platform or a phone call.
Finally, if a patient asks for a call, honor that request. Here are phrases to help you make the switch smoothly:
Transition 1: "I want to give this the attention it deserves. Can I call you in the next 15 minutes?"
Transition 2: "This is an important topic. I think a quick call would help us resolve it faster. What time works for you?"
Transition 3: "I appreciate you sharing this. For your privacy and to give you the best help, let me call you directly."
Transition 4: "I want to make sure we handle this the right way. Would a phone call in the next hour work for you?"
Transition 5: "This conversation is important to me, and I think we can solve it faster by phone. I will call you at [time]."
Knowing what to say matters. Knowing what not to say matters just as much. These common mistakes can turn a manageable issue into a serious problem.
Once your team masters the basics, these advanced techniques can lift their skills to the next level. Each one works best when layered on top of the five-step framework.
Empathy is more than a nice word. It is a tool that can shift the direction of a conversation in seconds. In text, it takes extra effort because you cannot rely on facial expression or vocal warmth.
There is a key difference between empathy and sympathy. Sympathy says, "I feel bad for you." Empathy says, "I understand what you are going through." In patient de-escalation techniques, empathy is the stronger move. It puts you beside the patient, not above them.
Try the emotional labeling method. Name the feeling you see in the message. "It sounds like you are feeling overlooked," or "I can sense your frustration," shows the patient you are paying attention. This simple act often reduces tension by half.
Mirroring the patient's own words can also help, but use it with care. If a patient says, "I feel like nobody cares," you might reply: "I hear that you feel like nobody cares, and I want to change that." This builds a connection without sounding like a script.
Here are empathy-focused scripts:
Script 1: "I can tell this has been really hard for you. I want to help."
Script 2: "It sounds like you have been dealing with this for a while. That is not okay, and I am going to work on it."
Script 3: "I hear you, and your feelings are valid. Let me see what I can do right now."
Script 4: "I understand how this could feel unfair. Let us work through it together."
Some patients will ask for things your practice cannot deliver. Saying no without damaging the relationship is a skill. The key is to offer what you can while being honest about what you cannot.
Start with what is possible. Instead of "We can't do that," try "Here is what we are able to offer." This frames the reply around a positive action. Patients hear a solution, not a wall.
Set clear boundaries with kindness. If a patient demands a same-day appointment and none exist, be direct but warm: "I wish I could fit you in today, but our schedule is full. I have a spot open tomorrow at 9 a.m. Can I book that for you?"
Managing expectations early prevents conflict later. If wait times are long or a referral takes days, tell the patient up front. This honest approach reduces the chance of an angry follow-up.
Scripts for boundary-setting:
Script 1: "I understand this is urgent for you. The earliest I can offer is [date/time]. I have reserved that spot for you."
Script 2: "I wish I could make that happen. Here is what I can do instead."
Script 3: "I want to be upfront with you. This process usually takes [timeframe]. I will keep you updated along the way."
Script 4: "I hear your request. While we are not able to do [X], we can offer [Y]. Would that work for you?"
There is a line between a frustrated patient and an abusive one. Your team needs to know where that line is and what to do when someone crosses it. A zero-tolerance policy for threats and personal attacks protects your staff.
The first response should still be professional. Acknowledge that the person is upset, but set a clear boundary. "I want to help you, but I need our conversation to stay respectful" is direct without being hostile.
If the language continues, involve management. Document every message. In some cases, the practice may need to end the text exchange or even the patient relationship. These choices should follow your written policy.
Know when to end the conversation. If a patient refuses to engage without insults, a final message like "I understand you are upset. I am not able to continue this conversation over text, but I want to help. Please call us at [number] so we can speak directly." This keeps the door open while protecting your team.
Firm boundary scripts:
Script 1: "I understand you are upset. I want to help, but I need us to communicate respectfully so I can assist you."
Script 2: "I hear your frustration. I am not able to continue if the language is hurtful. Let us try a phone call instead."
Script 3: "Your concern is valid. To give you the best support, I need to move this to a call with our manager. They will reach out shortly."
A protocol removes the stress of deciding what to do in the moment. When your team has a written plan, they can act fast and stay consistent. Building this protocol does not have to be complex.

Even the best scripts fall flat without proper training. Your staff needs practice, feedback, and ongoing support to handle tough text exchanges with confidence.
When your team feels equipped and backed up, they show up with more calm and more care. That mindset reaches patients in every message they send.
Here is a surprising truth. Patients who have a problem that gets resolved well often become more loyal than patients who never had an issue at all. This is called the service recovery paradox, and it is real.
When a patient complains, and your team responds with speed, empathy, and a clear fix, something shifts. The patient sees that you care. They feel valued. That moment of recovery can turn a critic into your biggest advocate.
After the issue is resolved, follow up with a check-in. Ask the patient if everything is okay. This one extra step shows that their experience matters beyond the immediate fix. It also opens the door for feedback that your practice can use to improve.
Track your recovery efforts. How many complaints came in this month? How many were resolved on the same day? How many patients returned after a difficult exchange? These numbers reveal how well your patient dissatisfaction management is working.
Turn complaint data into action. If billing issues keep coming up, maybe your billing process needs a closer look. If scheduling complaints are frequent, it may be time to review your booking system. Every pattern in your complaint data is an opportunity to get better.
The practices that excel at this do not fear complaints. They welcome them as chances to strengthen the bond with their patients. That mindset, backed by the skills and tools in this guide, is what sets great practices apart.
The right tools make difficult conversations easier to manage. Technology cannot replace human empathy, but it can support your team in critical moments.
Message templates and canned responses are a starting point. When a heated message comes in, your staff can pull up a pre-approved reply and customize it in seconds. This cuts down response time and reduces the risk of saying the wrong thing in the moment.
Team collaboration features matter, too. Look for a platform that lets staff tag a supervisor or loop in a colleague without the patient seeing the internal discussion. This behind-the-scenes teamwork leads to better, more thoughtful replies.
Escalation alerts are another key feature. Some platforms can flag messages with urgent language or negative sentiment. These alerts help your team catch hot issues before they get worse. Routing complex messages to the right person saves time and frustration.
Integration with your EMR gives your team full context when they reply. If a staff member can see the patient's visit history, billing notes, and past messages all in one view, they craft a better response.
A platform like Curogram offers these features along with HIPAA-compliant texting, which keeps every difficult exchange secure. For a closer look at the tools available, check out our patient texting software comparison guide.
Automation also plays a role. Smart routing can send billing questions straight to your billing team and clinical concerns to a nurse. This means the patient gets a faster, more accurate reply from the person best equipped to help.
Difficult patient conversations over text are part of running a modern medical practice. They will not go away. But with the right framework, they become manageable and even productive.
The core process is simple. Pause before you reply. Validate what the patient feels. Take responsibility when it fits. Offer a clear solution. Then follow through. These five steps, practiced over time, will change how your team handles every tough moment.
Skills grow with use. The more your staff practices these techniques, the more natural they become. Scripts give your team a starting point, but real confidence comes from training, support, and experience.
Every complaint is a chance to build a stronger relationship. When a patient sees that your team listens, responds with care, and follows through, their trust deepens. That trust keeps them coming back and telling others about your practice.
Take the next step. Build your protocol, train your team, and equip them with tools that support their best work.
If you are ready to see how the right platform can help, schedule a demo to explore what is possible for your practice.
Frequently Asked Questions
Staff should pause before replying, then acknowledge the patient's frustration with empathy. A simple phrase like "I hear you, and I want to help" goes a long way.
After validating their feelings, offer a specific next step with a timeline so the patient knows action is being taken.
Text removes vocal tone and body language, which carry most of the emotional meaning in a conversation. Without those cues, messages are easy to misread. Patients may also be more blunt in text, and delayed replies can make frustration grow before you even have a chance to respond.
Start with a written policy that defines complaint types, escalation tiers, and response time goals. Build a library of approved response templates for common situations. Train your team on the protocol through role-playing, then review and update the guidelines at least twice a year.
Research shows that patients whose problems are resolved quickly and with care often become more loyal than those who never had an issue. This is the service recovery paradox. A thoughtful response to a complaint signals that your practice values the relationship.
Some topics, like clinical concerns, legal issues, or escalating hostility, need the richness of a live voice.
Continuing these over text can lead to more confusion, increased risk, and a worse patient experience. Offering a phone call shows the patient you care enough to give the issue your full attention.

💡 Professional text communication in healthcare refers to the use of secure, HIPAA-compliant patient texting to manage appointments, share...
💡Secure, HIPAA-compliant texting is the future of healthcare communication. Transform your workflows with enterprise secure medical texting today.

💡 Medical practices improve daily workflows most effectively by using HIPAA-compliant 2-way texting to replace manual phone calls, rather than...