12 Actionable Strategies for How to Improve Medical Billing Process
In the complex ecosystem of healthcare, the financial health of your practice is just as critical as the well-being of your patients. The medical...
The medical billing process is a foundational system within any healthcare practice, responsible for converting patient services into financial reimbursement. A methodical approach to this process is essential for maintaining the financial health, operational efficiency, and regulatory compliance of a medical practice. An error at any point in the workflow can result in claim denials, payment delays, and significant impacts on revenue. This article explains the 12 core medical billing process steps, offering a clear framework for healthcare providers, office administrators, and billing specialists. By examining each stage, from initial patient contact to final account reconciliation, you can identify areas for improvement and ensure a more predictable revenue cycle.
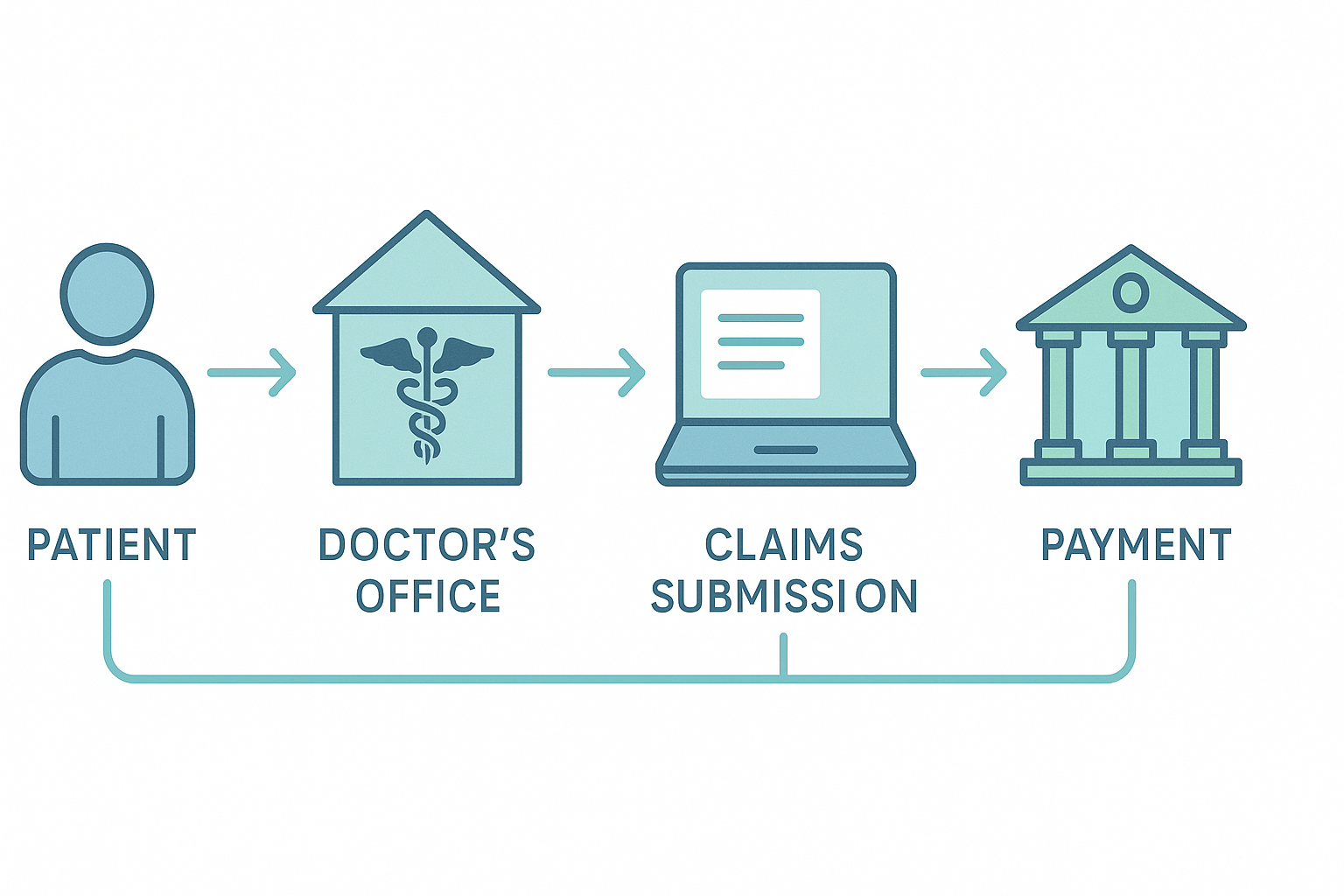
At its most basic level, the medical billing process functions as the communication channel between a healthcare provider and a patient's insurance company. This entire workflow, often called the Revenue Cycle Management (RCM), starts when a patient first makes an appointment and ends only when the provider has received full payment for all services. It involves a coordinated effort between three key parties: the Patient (who receives the care), the Provider (the physician, clinic, or hospital), and the Payer (the insurance company or a government body like Medicare/Medicaid). A successful process relies on accurate and timely data exchange among all three.
Implementing the medical billing process steps with care and precision is crucial for the stability of a modern healthcare practice. A well-run billing operation has a direct positive effect on nearly every aspect of the organization.
A functional understanding of the medical billing process requires knowing the function of each stage. Here is a breakdown of the 12 steps that form a successful revenue cycle.
The process begins here, before the patient arrives for their appointment. During scheduling and preregistration, the front office collects the foundational demographic and insurance data that will be used to build the future claim.
After collecting the patient's insurance information, it must be verified. This step confirms that the patient's coverage is active for the date of service and clarifies the details of their benefits.
This is the point where the clinical service is documented for billing purposes. During the visit, the physician records all diagnoses made and procedures performed in the patient's medical record.
Medical coding involves translating the provider's notes on diagnoses and procedures into standardized alphanumeric codes. This is one of the most technical medical billing process steps and requires specialized knowledge.
The coded information is entered into the billing system to create a formal claim. This claim is then "scrubbed," a term for a final audit to catch errors before it is sent to the payer.
Once the claim has been created, coded, and scrubbed, it is submitted to the insurance company for reimbursement.
When the payer receives the claim, they begin the adjudication process. This is the formal review where the insurance company decides whether to pay, deny, or reject the claim.
After adjudication, the payer sends payment to the provider along with a remittance document—either an Explanation of Benefits (EOB) or an Electronic Remittance Advice (ERA)—that details the payment decisions. The payment posting team then applies these payments to the correct patient accounts.
If a claim is denied, the process is not complete. Denial management involves investigating the reason for the denial and, when appropriate, appealing the payer's decision.
After the insurance company's portion has been paid, any remaining balance (such as a copay, deductible, or coinsurance) is billed to the patient.
This step focuses on collecting the outstanding balance directly from the patient.
The final step is the ongoing analysis of billing data. By tracking key metrics, a practice can monitor the performance of its revenue cycle and find opportunities to improve.
There isn't a universally "best" medical billing process, as the right model depends on a practice's specific situation, including its size, specialty, and available resources. The most common approaches are:
Technology is critical for an efficient billing workflow. Essential platforms include:
Every practice encounters billing challenges. The most frequent include:
The procedure in medical billing is a sequence of steps designed to secure payment for healthcare services. It begins with patient registration and insurance verification, moves to medical coding and claim creation, and then to claim submission. After the insurance company processes the claim, the final steps include posting the payment, billing the patient for their share, and analyzing the results.
The core steps in the billing process are: 1) Patient Registration, 2) Insurance Verification, 3) Encounter & Charge Capture, 4) Medical Coding, 5) Charge Entry & Scrubbing, 6) Claim Submission, 7) Payer Adjudication, 8) Payment Posting, 9) Denial Management, 10) Patient Billing, 11) Collections, and 12) Reporting.
The best process for medical billing depends on the practice. Smaller clinics often find outsourcing to a specialized company to be the most efficient. Larger healthcare systems may have the resources to maintain a high-performing in-house team. The best process is always one that is well-documented, uses technology effectively, and is focused on accuracy at every step.
CPT stands for Current Procedural Terminology. It is a set of medical codes used to report medical, surgical, and diagnostic procedures and services to payers. Within the medical billing process, CPT codes communicate to the insurance company exactly what services a provider performed.
The medical billing process is a critical business function that directly determines the financial viability of a healthcare practice. By applying a systematic approach to each of the 12 core medical billing process steps, providers can create a more stable and predictable revenue cycle. From the front desk to the back office, focusing on accuracy and efficiency at each stage will reduce errors, improve cash flow, and lead to a better financial experience for patients.

In the complex ecosystem of healthcare, the financial health of your practice is just as critical as the well-being of your patients. The medical...

Expert radiology medical billing services and precise radiology billing and coding are absolutely vital for the financial strength and operational...

In the complex and ever-evolving landscape of healthcare, efficient financial management is the backbone of a thriving practice. For many, the most...