The Medical Billing Process: Exploring the 12 Core Steps
The medical billing process is a foundational system within any healthcare practice, responsible for converting patient services into financial...
11 min read
Alvin Amoroso : July 4, 2025

In the complex and ever-evolving landscape of healthcare, efficient financial management is the backbone of a thriving practice. For many, the most significant hurdle lies in mastering the nuances of the revenue cycle, specifically medical billing. Improper billing practices don't just lead to delayed payments; they can result in outright revenue loss, compliance risks, and administrative chaos. This is precisely why arming your practice with the most effective medical billing tips and tricks is not just beneficial—it's essential for survival and growth.
This comprehensive guide goes beyond the basics. We will delve into 11 actionable strategies designed to optimize your billing process, minimize common errors, and secure your financial foundation. Whether you are managing a small independent practice or a larger healthcare facility, these insights will provide a clear roadmap to enhancing your revenue stream and operational efficiency. We will cover everything from leveraging technology and understanding payer-specific requirements to empowering your staff with continuous education. By implementing these expert-backed tips, you can transform your billing department from a cost center into a powerful revenue-generating engine.
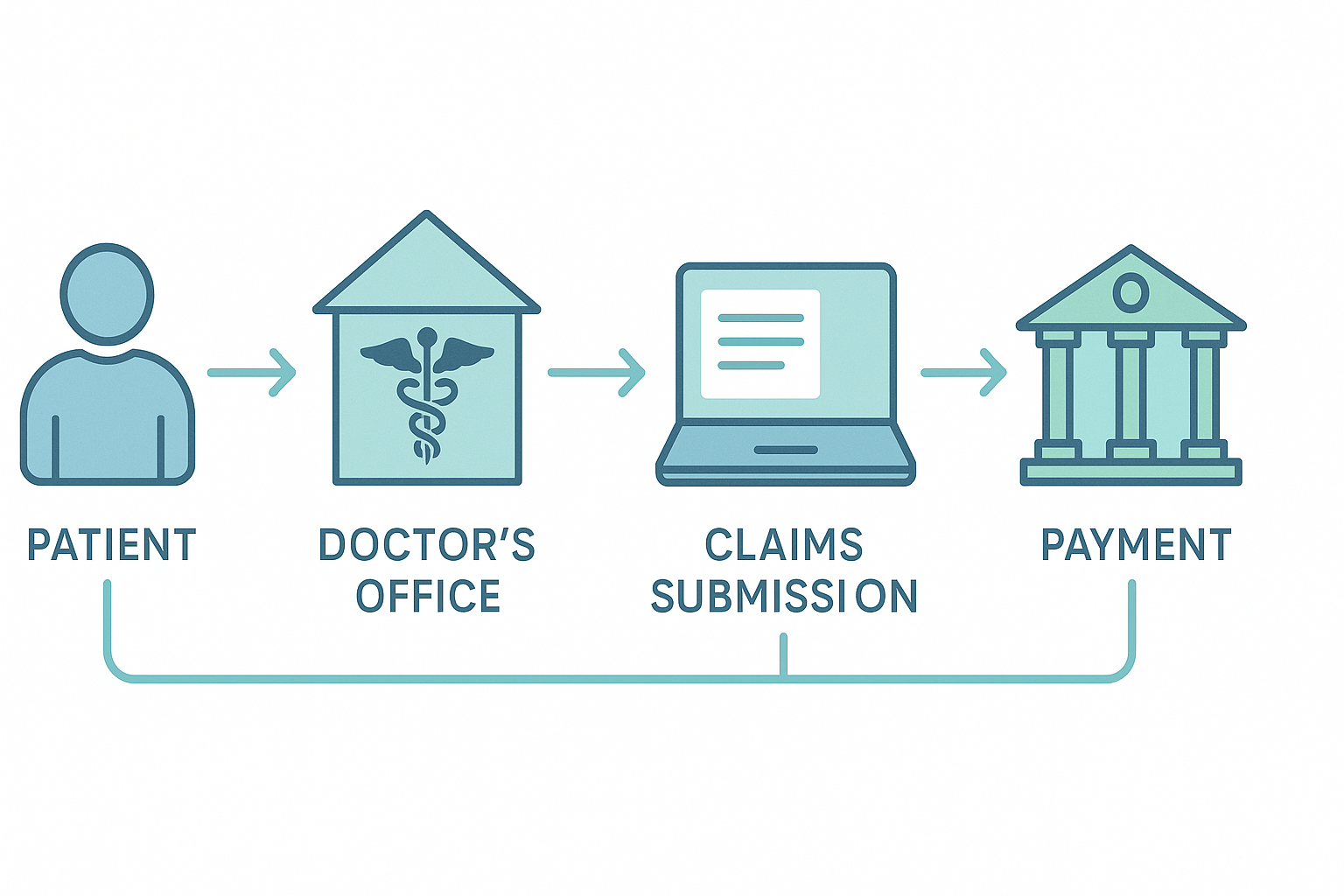
Before we dive into the specific tips, it's crucial to understand what's at stake. Medical billing is the intricate process of submitting and following up on claims with health insurance companies in order to receive payment for services rendered by a healthcare provider. It's the final, critical step in the patient care journey that ensures your practice is compensated for its hard work.
However, this process is fraught with challenges. From complex coding systems like ICD-10 and CPT to the varying rules of thousands of different insurance payers, the margin for error is slim. A single mistake—a mistyped digit in a patient's policy number, an incorrect code, or a missed filing deadline—can lead to a claim denial. According to industry reports, denial rates can range from 5% to over 10%, and a significant portion of these denied claims are never successfully reworked or resubmitted. This translates directly to lost revenue.
Therefore, implementing robust medical billing and coding tips and tricks is the most proactive measure you can take to protect your practice's financial health and ensure long-term stability.
One of the most effective medical billing tips and tricks happens before a patient even sees a provider. The root cause of a vast majority of claim denials is inaccurate or incomplete patient information collected at the front desk. A proactive, meticulous verification process is your first line of defense.
Your front-end staff must be trained to be detectives. They should verify every piece of information during patient registration and check-in. This includes:
By investing time and resources in front-end accuracy, you prevent countless downstream problems, reduce denials, and accelerate your payment cycle significantly.
In today's digital age, relying on manual processes for medical billing is like navigating a highway on a bicycle—it's slow, exhausting, and incredibly risky. Technology is arguably the most powerful tool in your arsenal of medical billing tips and tricks.
Investing in a modern Practice Management (PM) and Electronic Health Record (EHR) system is paramount. These systems should not operate in silos; they must be fully integrated. An integrated system allows for a seamless flow of information from the clinical side (EHR) to the administrative side (PM). When a provider documents a patient encounter in the EHR, the relevant codes and data should automatically populate a claim form in the PM system.
Key technological tools to implement include:
Automating these processes frees up your billing staff from tedious administrative tasks, allowing them to focus on more complex issues like denial management and detailed financial analysis. For practices looking to improve efficiency, exploring options like our advanced revenue cycle management services can provide an integrated solution.
A "clean claim" is a claim that is received and processed by a payer without needing any additional information or correction. The goal of your billing department should be to achieve a clean claim rate of 95% or higher. This is central to any effective list of medical billing tips and tricks.
Achieving this requires a multi-pronged approach that builds on the previous points:
Submitting clean claims accelerates your cash flow, reduces the administrative burden of rework, and builds a positive reputation with insurance payers.
Despite your best efforts, some claims will inevitably be denied. The difference between a financially successful practice and one that struggles is how it manages these denials. A passive approach is a recipe for revenue loss. You need an aggressive, data-driven denial management strategy.
This involves several key steps:
An effective denial management system turns a negative event into a positive learning opportunity that strengthens your entire revenue cycle.
The world of medical billing and coding tips and tricks is not static. Coding guidelines are updated annually, payer policies change quarterly, and new regulations are introduced constantly. A team that doesn't receive ongoing training will quickly fall behind, leading to an increase in errors and denials.
Investing in continuous education is one of the highest-return investments a practice can make. This should include:
A well-educated team is a confident and effective team, forming the human firewall against revenue leakage. For those looking for structured learning, consider our comprehensive medical billing courses.
You cannot improve what you do not measure. Running a billing department without tracking KPIs is like flying a plane without an instrument panel. Analyzing your performance data provides the critical insights needed to make informed business decisions.
Your practice should be regularly tracking and reviewing these essential KPIs:
Reviewing these KPIs in monthly meetings with your billing team and management will help you identify trends, celebrate successes, and pinpoint areas that need immediate attention.
While insurance payers account for the bulk of your revenue, patient responsibility (co-pays, deductibles, and co-insurance) is a rapidly growing portion of the pie. An often-overlooked area of medical billing tips and tricks is how you communicate with and collect from your patients.
Your patient statements should be clear, simple, and easy to understand. A confusing bill filled with medical jargon and complex codes is likely to be ignored. Consider these best practices:
Provider credentialing is the process of verifying a provider's qualifications to ensure they are eligible to participate in a payer's network. If a provider's credentialing is not complete or has expired with a particular insurance plan, any claims submitted for their services will be denied.
This is a critical, yet often poorly managed, administrative function.
A chart audit is an internal or external review of clinical documentation and medical billing records to ensure accuracy, compliance, and proper reimbursement. Regular audits are a powerful tool for identifying and correcting potential issues before they become major problems.
Audits can help you:
Performing quarterly audits on a small sample of charts (e.g., 5-10 per provider) is a manageable and highly effective strategy.
One of the biggest breakdowns in the revenue cycle occurs when the clinical staff (doctors, nurses) and the administrative staff (billers, coders) operate in separate universes. Fostering a culture of open communication and collaboration is one of the most impactful, yet least technical, medical billing and coding tips and tricks.
When coders have questions about a provider's documentation, they should feel comfortable approaching the provider for clarification without fear of being dismissed. When providers are unsure about the documentation requirements for a new procedure, they should know who to ask on the billing team.
Schedule brief, regular meetings between the two teams to discuss common issues, review denial trends, and share updates. This collaboration ensures that everyone understands their role in the revenue cycle and is working toward the same goal: getting the practice paid accurately and efficiently for the excellent care it provides.
Finally, one of the most strategic medical billing tips and tricks is to honestly assess your practice's capabilities. For many small to medium-sized practices, managing the sheer complexity of medical billing in-house can be overwhelming and economically inefficient. The costs of salaries for expert staff, sophisticated software, continuous training, and the administrative overhead can be substantial.
Partnering with a professional medical billing company can be a game-changing decision. A dedicated billing service offers several advantages:
When considering outsourcing, look for a partner, not just a vendor. Find a company that offers transparency, detailed reporting, and becomes an integrated part of your team. This can be the ultimate trick to unlocking your practice's full revenue potential.
The best way to learn medical billing is through a combination of structured education and hands-on experience. Start by enrolling in a reputable certificate or diploma program from an accredited institution. These programs teach the fundamentals of medical terminology, anatomy, coding systems (ICD-10, CPT), and insurance regulations. Upon completion, seeking a certification like the Certified Professional Biller (CPB) from the AAPC validates your knowledge. Following formal education, gaining experience in an entry-level position is crucial. This real-world application is where you will learn payer-specific rules, practice management software, and the critical art of denial management.
The most common reasons for claim rejections are simple clerical errors and missing or incorrect patient information. This includes typos in a patient's name or policy number, an incorrect date of birth, or missing insurance information. Another very frequent cause for rejection is a mismatch between the procedure code and the diagnosis code. Claims are also commonly rejected for being filed after the payer's timely filing deadline or for lacking the required pre-authorization for a service. Implementing a thorough front-end verification process is the single most effective way to reduce these common rejections.
The biggest challenge in medical billing is keeping up with the constant and complex changes across the industry. This includes annual updates to thousands of medical codes, frequent changes in policies from hundreds of different insurance payers, and evolving federal and state regulations. This constant flux requires continuous education and vigilance. Managing claim denials effectively is a close second, as it demands analytical skills to identify root causes and a persistent, organized approach to appeal and recover revenue that would otherwise be lost.
The golden rule in medical coding and billing is: "If it wasn't documented, it wasn't done." This principle underscores that all billed services must be supported by thorough and accurate documentation in the patient's medical record. Coders and billers can only code for the procedures, diagnoses, and services that the provider has clearly documented. This rule is critical for compliance, as it forms the basis of proof during an audit. Accurate documentation not only ensures proper payment but also protects the practice from allegations of fraud and abuse.
The medical billing process is a foundational system within any healthcare practice, responsible for converting patient services into financial...

In the complex ecosystem of healthcare, the financial health of your practice is just as critical as the well-being of your patients. The medical...

Expert radiology medical billing services and precise radiology billing and coding are absolutely vital for the financial strength and operational...