Simplifying Virtual Visits in Veradigm with Telehealth
💡 Telehealth helps imaging centers work faster and smarter. Virtual visits that Veradigm users rely on cut down delays and improve patient care....
14 min read
Jo Galvez
:
Updated on January 10, 2026

Table of Contents
Every empty appointment slot represents lost revenue that can never be recovered. Imaging centers run on tight margins where schedule disruptions directly impact the bottom line. A single wave of cancellations can erase an entire day's profit.
Traditional coordination methods create preventable inefficiencies throughout the patient journey. Phone tag delays pre-procedure screening. Verbal instructions lead to prep failures. Follow-up appointments get postponed indefinitely. Each friction point costs time and money.
Most imaging leaders understand these problems but struggle to find practical solutions. Adding more front desk staff doesn't solve coordination issues. Expanding facility space costs millions. Extending hours increases overhead without addressing root causes.
Expand access Veradigm telehealth offers a different approach that targets the source of inefficiency. Virtual screening catches problems before patients travel to the facility. Video consultations clarify prep requirements through visual demonstration. Remote follow-ups happen on patient schedules rather than center availability.
These improvements show up immediately in operational metrics. Schedule reliability increases when patients arrive properly prepared. Modality utilization climbs as cancellations drop. Administrative costs decrease as phone volume falls.
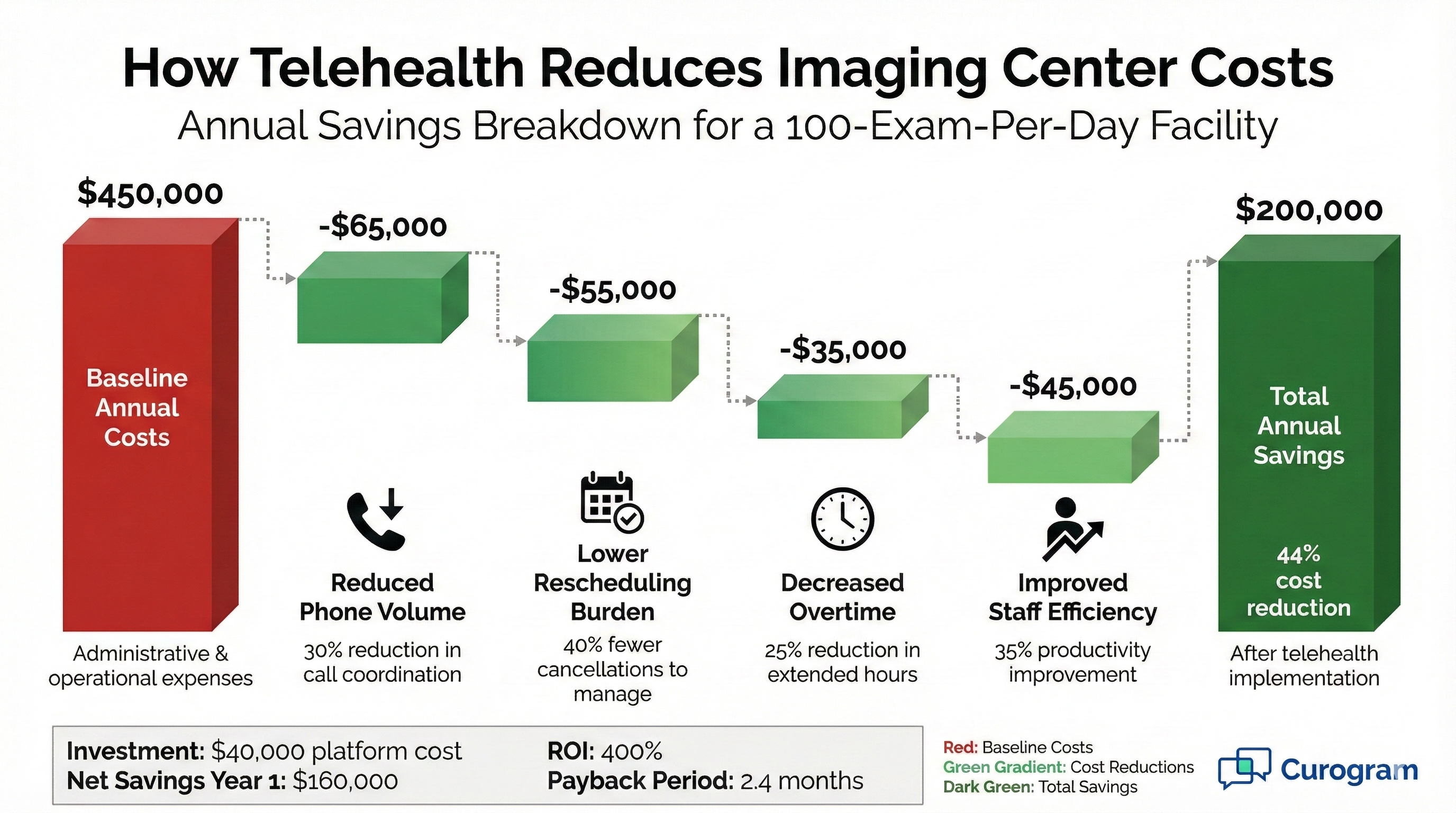
The financial impact becomes clear within the first quarter of implementation. Centers may see 30-40% reductions in prep-related cancellations. Staff productivity can improve by 25% as coordination becomes more efficient. Patient satisfaction scores rise alongside operational performance.
This blog examines the specific ways telehealth creates telemedicine ROI for imaging centers. We'll explore revenue protection, throughput improvements, cost reduction, and scaling advantages. You'll see concrete examples of how hybrid care workflow transforms daily operations while strengthening financial performance.
Imaging centers run on tight margins. Every appointment slot represents potential revenue. When schedules break down, profits suffer. Telehealth fixes the weak points that cause these breakdowns.
Traditional workflows rely heavily on manual coordination. Staff make repeated calls to prep patients and confirm details. This approach wastes time and creates gaps where problems hide. Issues only surface when patients arrive unprepared.
Virtual care transforms these pain points into strengths. Pre-visit screening happens efficiently through scheduled video sessions. Follow-up conversations occur faster. The entire patient journey becomes more predictable and less prone to costly surprises.
For Veradigm users, these improvements integrate smoothly into existing systems. Staff don't need to learn completely new processes. The hybrid care workflow simply enhances what already works. ROI appears quickly because adoption happens naturally.
Every completed exam generates revenue. Every cancellation or no-show represents lost income. The difference between 85% and 95% completion rates significantly impacts annual profitability.
Telehealth pushes completion rates higher by addressing root causes of failures. Better prep education reduces day-of surprises. Virtual screening catches medical contraindications early. Convenient follow-up options reduce no-shows for results discussions.
Consider a practice averaging 800 billable exams monthly. Improving completion rates by just 5% adds 40 exams per month. At an average reimbursement of $300, that's $12,000 in additional monthly revenue. The annual impact reaches $144,000.
These gains require no new equipment or facility expansion. The same MRI scanner, CT suite, and ultrasound rooms generate more revenue. Telemedicine ROI becomes obvious when you measure throughput improvements against implementation costs.
MRI and CT scanners represent major capital investments. Every hour these machines sit idle wastes money. Maximum utilization requires reliable patient flow without gaps or delays.
Last-minute cancellations create the worst kind of waste. The slot goes unfilled because there's no time to reschedule. Staff processed intake paperwork. The patient made arrangements to come. Everyone lost time and the facility lost revenue.
Virtual pre-screening prevents these losses. Problems surface days in advance instead of on appointment day. Staff can reschedule and fill the slot with another patient. Expensive equipment stays productive instead of sitting empty.
IR procedures benefit even more from this approach. These high-value appointments require extensive prep and carry greater revenue impact.
Fast patient turnover maximizes daily appointment capacity. Delays between exams reduce total volume. Even 15 minutes of slack per slot adds up across a full schedule.
Traditional workflows create unnecessary delays. Staff wait for patient callbacks to confirm details. Clinical questions need time-consuming coordination. These small pauses accumulate into significant throughput losses.
Telehealth streamlines these interactions. Virtual pre-visits resolve questions efficiently. Patients arrive knowing exactly what to expect. Check-in moves faster. Exams start on time. The schedule flows smoothly without constant staff intervention.
This efficiency lets centers fit more appointments into each day. A practice might add two or three slots daily without extending hours. Over a year, that translates to hundreds of additional billable exams from the same resources.
Unprepared patients cost imaging centers thousands monthly. Failed exams waste time and resources. Revenue disappears when appointments don't convert to completed studies. Virtual care attacks this problem at its source.
Same-day cancellations inflict maximum financial damage. The slot can't be refilled. Staff already invested prep time. The patient interrupted their schedule. Everyone loses, but revenue takes the biggest hit.
Many cancellations stem from preventable issues. Patients didn't fast properly. They took medications they should have stopped. Their medical history revealed contraindications. These problems were always present but remained hidden until too late.
When you expand the access Veradigm telehealth provides, screening moves earlier in the patient journey. Virtual sessions catch red flags days before scheduled appointments. Staff identify problems while time remains to address them or reschedule appropriately.
This proactive approach protects revenue across all modalities. CT scans proceed without contrast complications. MRI appointments happen despite metal implant concerns. IR procedures go forward with proper anticoagulation management. Each prevented cancellation preserves $300 to $5,000 in revenue.
Some patients shouldn't receive certain exams at all. Medical conditions or allergies create absolute contraindications. Discovering these issues on appointment day wastes everyone's time.
Virtual screening reviews medical history thoroughly before booking. Clinicians spot potential problems early. Alternative imaging options are arranged promptly. The right exam gets scheduled the first time instead of after failed attempts.
Ensuring Patients Receive Accurate Prep Instructions
Prep failures waste enormous resources. Patients arrive having eaten when they needed empty stomachs. They took medications that interfere with procedures. They didn't follow clear instructions because they never truly understood them.
Phone-based instruction creates comprehension gaps. Patients nod along during calls but miss critical details. They can't ask questions that only occur later. Written instructions sit unread or misinterpreted.
Virtual prep sessions solve these communication failures. Staff demonstrate requirements visually. Patients ask questions immediately when confusion arises. Written summaries sent afterward reinforce verbal instruction. Understanding improves dramatically.
Better preparation directly protects revenue. Fewer patients arrive in non-fasting states. Medication management follows protocols correctly. Exam success rates climb. The hybrid care workflow ensures patients come ready to complete their studies.
IR procedures demand detailed preparation. Patients must manage anticoagulation, understand sedation requirements, and arrange transportation. These complex instructions overwhelm many patients when delivered by phone.
Telehealth breaks complex prep into clear, visual steps. Clinicians share screens showing prep timelines. They review medication adjustments in detail. Patients see exactly what success looks like. This thoroughness prevents costly IR cancellations.
Maintaining Predictable Daily Volume
Revenue stability requires volume predictability. Wild swings in daily appointments create financial uncertainty. Staff schedules become inefficient. Equipment utilization varies unpredictably.
Better prep compliance creates stable volume patterns. Completion rates remain consistently high. Cancellations become rare exceptions instead of frequent disruptions. Financial planning grows more accurate.
This predictability improves operational efficiency across the organization. Staffing levels match actual needs. Supply ordering becomes more accurate. Cash flow steadies. Management makes better decisions based on reliable volume data.
For multi-location practices, standardized virtual screening creates uniform performance across sites. One facility doesn't struggle while another thrives. Consistent processes produce consistent results. Enterprise-wide telemedicine ROI becomes measurable and predictable.
Equipment sits at the heart of imaging center profitability. These expensive assets must stay productive to justify their cost. Empty scan time equals wasted investment. Incorporating telehealth helps maximize every dollar spent on imaging equipment.
Pre-exam delays eat into productive scan time. Staff wait for clinical clearance calls. Questions about prep take days to resolve. These delays push appointments back and reduce daily capacity.
Traditional phone coordination creates these bottlenecks naturally. Staff leave voicemails that go unreturned. Patients call back when staff are busy with others. Simple questions stretch across multiple days through asynchronous communication.
Virtual consultations collapse these timelines dramatically. A 15-minute video session resolves what might take a week of phone tag. All questions get answered in one interaction. Decisions happen immediately. Appointments proceed without unnecessary delays.
This acceleration directly improves throughput. Patients move through their care journey faster. Appointment scheduling becomes tighter. The same facility completes more exams monthly without adding hours or equipment.
High-risk patients often need physician clearance before imaging. This approval process can delay appointments by weeks. Patients wait while providers exchange information slowly through traditional channels.
Virtual platforms speed up these consultations significantly. Radiologists can review patient histories via video. They make clearance decisions during the session. Documentation happens immediately. Appointments get scheduled right away instead of after prolonged coordination.
Follow-up appointments often take weeks to arrange. Patients can't find convenient slots. Scheduling staff play phone tag, trying to coordinate. These delays slow down the entire care continuum.
When you expand access that Veradigm telehealth delivers, follow-ups happen faster. Virtual slots are more plentiful than in-person availability. Patients book convenient times immediately. Care keeps moving forward without lengthy pauses between steps.
Multi-site imaging networks struggle with inconsistent performance. One location achieves 95% utilization while another barely reaches 80%. These gaps indicate workflow problems that drain profitability.
Variability often stems from different communication approaches. Each site developed its own methods for patient coordination. Some techniques work better than others. But without standardization, best practices don't spread across the network.
Centralized virtual care eliminates this inconsistency. Every location uses the same screening protocols. Patient prep education follows identical steps. Follow-up processes match across all sites. Performance converges toward the highest standards.
This standardization produces measurable financial benefits. Weak performers catch up to strong ones. Total network utilization rises. Revenue increases without adding facilities. The hybrid care workflow creates organizational efficiency that compounds over time.
Virtual care platforms generate detailed performance metrics. Management can see completion rates, prep failure rates, and no-show percentages for each location. These numbers highlight which sites need improvement.
Data-driven management becomes possible when all sites use the same system. Leaders identify best practices from top performers. They implement those methods network-wide through standardized virtual workflows. Improvement happens faster because the data shows exactly what works.
MRI machines cost over $1 million. CT scanners run $200,000 or more. These assets must generate substantial revenue to justify their expense. Low utilization kills return on investment.
Every percentage point of utilization improvement matters significantly. A $1 million MRI operating at 75% instead of 70% capacity generates $50,000 more annual revenue. Across multiple machines, these gains become substantial.
Telehealth pushes utilization higher through multiple mechanisms. Fewer cancellations keep slots filled. Faster turnover fits more patients into each day. Better scheduling reduces gaps between appointments. All these improvements flow to the bottom line.
The financial impact scales with equipment value. High-cost modalities see the biggest dollar gains from utilization improvements. IR suites and advanced imaging equipment benefit most. But even basic ultrasound and X-ray operations gain meaningful efficiency.
Physical facilities have limited operating hours. Extending hours requires overtime pay and additional staffing. These costs quickly erode the value of extra appointments.
Virtual consultations happen outside standard facility hours without extra facility costs. Staff conduct evening or weekend prep sessions from home. Patients receive convenient service times. The practice expands access without expanding physical operations or paying overtime premiums.
Scheduling teams field hundreds of calls weekly. Patients ask basic questions about prep, timing, and location. Each call takes staff away from more valuable work. The time adds up to significant labor costs.
Virtual sessions replace many routine phone interactions. One scheduled video call handles what might require five or six phone conversations. Staff allocate time more efficiently. They help more patients with fewer total hours worked.
The cost savings prove substantial over time. A practice might reduce phone time by 15-20 hours weekly. That's nearly a full-time position's worth of labor redirected to higher-value activities. Annual savings can exceed $40,000 in reduced staffing needs.
Rescheduling failed appointments consumes enormous staff time. Coordinators must call patients, reach referring physicians, update systems, and find new slots. One cancellation can require 30 minutes of coordination work.
Better prep screening reduces these failures significantly. Fewer patients arrive unprepared. Cancellations drop. Staff spend less time fixing schedule problems and more time supporting successful appointments.
This efficiency gain becomes more valuable as volume grows. A center preventing 20 cancellations monthly saves 10 hours of rescheduling work. That time supports better patient service or allows staff reduction through attrition.
Patients value convenience highly. Long drives to appointments frustrate them. Taking time off work creates stress. Parking hassles add annoyance. These friction points harm the overall experience.
Virtual visits eliminate many common frustrations. Patients connect from home or work. They avoid traffic and parking issues. Appointment times fit better into busy schedules. This convenience translates directly into higher satisfaction scores.
Satisfied patients leave positive online reviews. These reviews influence where new patients choose to go. Strong ratings become a competitive advantage that drives organic growth. The telemedicine ROI includes improved reputation value.
Patients expect modern healthcare to include digital options. Practices offering telehealth meet these expectations. Those relying solely on phone and in-person care feel outdated. Meeting patient expectations builds loyalty and drives retention.
Confused patients don't follow through with care plans. They skip recommended follow-up imaging. They delay necessary procedures. This non-compliance hurts both patient outcomes and facility revenue.
When you expand access Veradigm telehealth enables, patient understanding improves. Virtual face-to-face conversations create clarity. Patients ask questions freely. They leave sessions confident about next steps.
Better compliance drives repeat business naturally. Patients complete their full imaging series. They return for annual screenings. They follow through on physician recommendations. This steady patient flow provides predictable long-term revenue.
Consumer video platforms like Zoom or FaceTime don't meet healthcare security requirements. Using them for patient consultations violates HIPAA. Many practices unknowingly create compliance risks through improper technology choices.
Healthcare-specific telehealth platforms eliminate these risks. End-to-end encryption protects every session. Business associate agreements provide legal coverage. All communications remain compliant without extra staff effort.
This protection has real financial value. HIPAA violation fines start at $100 per record and can reach millions. Proper telehealth implementation prevents these catastrophic costs. The compliance benefit alone justifies the investment for many organizations.
Large imaging networks need visibility into all patient interactions. Compliance teams require detailed records. IT departments must track system access and usage. These oversight needs become complex across multiple locations.
Enterprise telehealth platforms provide comprehensive logging. Every session generates secure records. Administrative teams can audit interactions when needed. This transparency supports governance requirements while protecting patient privacy.
Strong audit capabilities reduce organizational risk significantly. Management can demonstrate compliance to regulators. Problems get identified quickly through routine monitoring. The hybrid care workflow stays secure without sacrificing efficiency.
Multi-site expansion typically demands proportional staff increases. Each new location needs schedulers, coordinators, and administrative support. These labor costs compress margins and slow growth.
Centralized virtual care changes this equation. One team can handle prep screening and follow-up for multiple locations. Patients at different sites receive the same high-quality service. Staff productivity multiplies across the network.
This scalability improves as networks grow. A 10-location practice gains more benefit than a three-site operation. The telemedicine ROI compounds with organizational size. Larger networks achieve better returns on their technology investments.
Virtual workflows enable organizational restructuring. Tasks once scattered across locations can be centralized. Specialized staff become more efficient in handling their specific functions. Total headcount needs decrease even as patient volume grows.
Physical space limitations constrain many imaging centers. Waiting rooms fill up. Consultation rooms stay booked. Expansion requires expensive construction or leasing.
Virtual consultations free up physical capacity. Pre-visit screening happens remotely. Follow-up discussions don't need exam rooms. The same space serves more imaging patients because non-imaging interactions move online.
This efficiency delays or eliminates facility expansion costs. A practice might serve 20% more patients in the same space. That's $200,000 to $500,000 in construction costs avoided. The financial impact equals years of telehealth platform fees.
Small-practice telehealth platforms can't handle enterprise imaging volume. They slow down under heavy load. Performance becomes unreliable during peak periods. These limitations make them poor choices for busy imaging centers.
Curogram handles thousands of sessions daily across multiple facilities. The platform stays fast and responsive regardless of usage spikes. Staff maintain confidence in system reliability. IT teams avoid constant troubleshooting and performance complaints.
This reliability proves especially important for IR workflows. Complex procedures require detailed virtual prep sessions. Technical problems during these critical conversations waste time and frustrate patients. Stable, dependable technology protects the investment in virtual care.
High-volume capability also supports future growth. Practices don't outgrow the platform as they expand. The same system serves 5,000 monthly sessions as easily as 500. Scalability protects the technology investment over many years.
Stand-alone telehealth systems create integration headaches. Staff log into separate platforms. Information doesn't flow between systems. Duplicate data entry wastes time. These friction points undermine the efficiency gains telehealth should provide.
Curogram connects directly with Veradigm scheduling and documentation. Virtual appointments appear in the same calendar as in-person visits. Staff use familiar interfaces. Information entered once flows where needed automatically.
This integration reduces training time significantly. Staff already know how to use Veradigm. Adding virtual visits requires minimal new learning. Adoption happens quickly because the technology feels like a natural extension of existing workflows.
Fast adoption accelerates ROI achievement. Practices see benefits within weeks instead of months. Staff resistance stays low. The hybrid care workflow enhancement delivers value immediately without lengthy implementation delays.
Security can't be an afterthought in healthcare technology. Every virtual session involves protected health information. Weak security creates legal exposure that can destroy organizations financially.
Curogram employs end-to-end encryption for all communications. Sessions meet HIPAA and SOC 2 requirements without additional configuration. Enterprise IT teams maintain full oversight through comprehensive audit logs.
This security framework reduces compliance workload. IT doesn't need to build custom security measures. Audit trails are generated automatically. Compliance teams can verify protection measures easily during reviews.
Strong security also protects telemedicine ROI directly. Breaches cost millions in fines, legal fees, and reputation damage. Proper protection prevents these catastrophic losses. The platform pays for itself by avoiding a single serious security incident.
Single-site solutions don't scale well across networks. Each location becomes its own silo. Management loses visibility into overall performance. Best practices don't spread effectively between facilities.
Curogram provides enterprise-wide visibility and control. Leadership sees performance metrics across all locations. Standardized workflows ensure consistency. Central teams support multiple sites efficiently.
This organizational approach maximizes network-wide ROI. Weak performers improve through standardization. Strong performers set benchmarks that others follow. The entire organization operates more efficiently when all sites use proven methods.
Telehealth ROI shows up clearly in imaging center financials. Protected revenue from prevented cancellations. Lower costs through reduced administrative burden. Higher throughput from better workflow efficiency. These gains prove measurable and sustainable.
The investment required remains modest compared to returns. Platform fees typically cost less than one prevented high-value cancellation per month. Implementation happens quickly with minimal disruption. Benefits begin accumulating within weeks.
When you expand access with Veradigm's telehealth capabilities, multiple financial benefits compound together. Completion rates improve. Equipment utilization rises. Staff productivity increases. Patient satisfaction strengthens. Each gain reinforces the others.
Multi-location networks see especially strong returns. Standardized virtual workflows create consistency that improves network-wide performance. Weak sites catch up to strong ones. Total organizational efficiency rises significantly.
The competitive advantages extend beyond internal operations. Patients appreciate convenient care options. Positive reviews attract new volume. Modern service offerings differentiate the practice from competitors stuck in traditional models.
For Veradigm users specifically, the right platform makes implementation smooth. Curogram integrates seamlessly with existing workflows. Staff adoption happens naturally. Technical challenges stay minimal.
Security and compliance remain strong throughout. Enterprise-grade encryption protects all sessions. Audit trails support governance needs. IT teams maintain full visibility and control.
The hybrid care workflow this creates serves imaging centers well for years. Technology investments pay back through sustained operational improvements. Patient care quality rises alongside financial performance. Both goals advance together through smart technology adoption.
Book a Demo to See Curogram + Veradigm in Action.
Virtual pre-visit screening catches problems days before scheduled appointments instead of on the day of service. Staff can reschedule and fill slots with other patients when issues surface early. This prevents wasted scan time and lost revenue. Each prevented high-value cancellation can save $500 to $5,000 in protected revenue.
Larger networks gain more from standardized workflows across all facilities. One centralized team can handle virtual care for multiple locations efficiently. Performance gaps between sites close as everyone follows the same proven processes. The cost savings and efficiency gains multiply across more locations, creating stronger overall returns.
Fewer cancellations keep expensive scanners productive instead of sitting idle. Faster pre-visit coordination reduces delays between appointments. Better patient preparation means exams complete successfully the first time. These improvements let imaging centers fit more billable studies into each day using the same equipment.
One virtual session replaces multiple phone calls spread across days or weeks. Staff spend less time on repetitive administrative tasks. Patients understand instructions better through face-to-face visual communication. This efficiency reduces labor costs while improving outcome quality and patient satisfaction.
Most centers see measurable benefits within the first month of full implementation. Prevented cancellations and reduced administrative time create immediate financial impact. Patient satisfaction improvements and volume growth build over subsequent months. The total ROI typically exceeds platform costs within the first quarter of operation.

💡 Telehealth helps imaging centers work faster and smarter. Virtual visits that Veradigm users rely on cut down delays and improve patient care....
💡 Telehealth in Veradigm helps imaging centers handle pre-exam prep, post-visit consults, and patient coordination more easily. Fewer no-shows...
💡 Traditional telehealth platforms aren’t built for imaging center workflows, creating daily frustration for both staff and patients. Curogram...