12 Actionable Strategies for How to Improve Medical Billing Process
In the complex ecosystem of healthcare, the financial health of your practice is just as critical as the well-being of your patients. The medical...
8 min read
Alvin Amoroso : Updated on June 30, 2025

The financial health of any healthcare practice hinges on its ability to get paid for the services it provides. At the very heart of this process lies charge capture medical billing, a critical function that ensures every billable service is accurately recorded, coded, and submitted for reimbursement. Mastering this process is not just an administrative task; it's a fundamental strategy for optimizing the entire revenue cycle, preventing costly revenue leakage, and ensuring long-term financial stability.
This comprehensive guide will walk you through the nine essential pillars of a flawless charge capture system. We'll explore everything from the initial patient interaction to advanced auditing techniques, providing actionable insights to transform your billing process into a powerhouse of efficiency and accuracy.
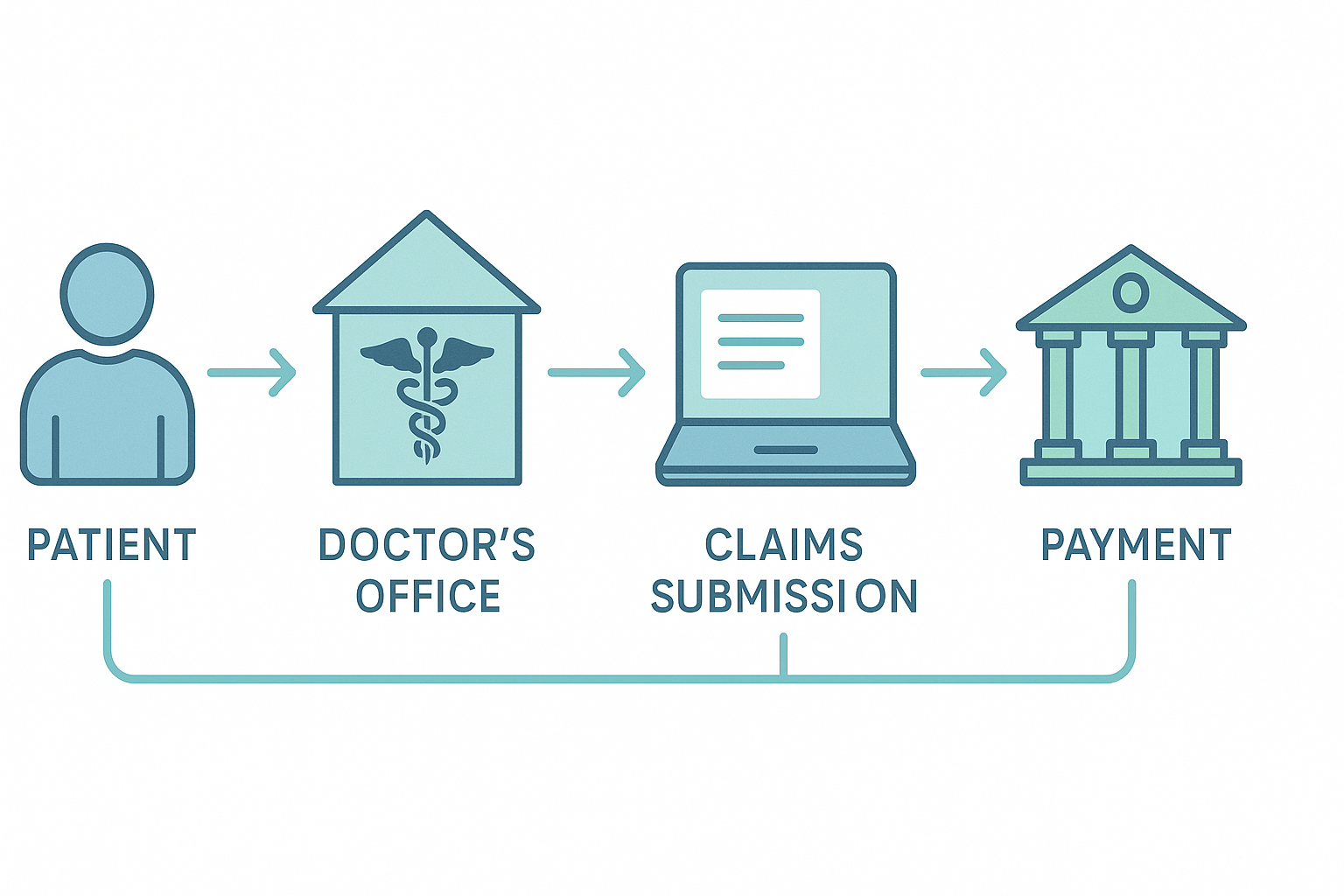
Before diving into the pillars, it's crucial to understand what is charge capture in healthcare at its core. Simply put, charge capture is the process of documenting services rendered to a patient and assigning a monetary value to them, which then becomes a "charge" on their account. This process serves as the bridge between the clinical side of medicine (patient care) and the financial side (billing and reimbursement). When a physician performs a consultation, a nurse administers a vaccine, or a technician runs a lab test, each action must be "captured" to ensure the facility is compensated. A breakdown in this critical first step of the charge capture revenue cycle means lost revenue, pure and simple.
The charge capture process begins the moment a patient schedules an appointment. Accurate and complete patient registration is the bedrock upon which all subsequent billing activities are built. This isn't just about getting a name and phone number; it's about meticulously collecting and verifying every piece of demographic and insurance information.
The first 1-2 sentences after each heading answer the topic completely and include the keyword. Every detail, from the correct spelling of a patient's name to the active policy number and group ID, is vital. A single typo or outdated piece of information can lead to an immediate claim denial, forcing your staff into a time-consuming rework process and delaying payment. Establishing a standardized, multi-point verification protocol during registration is the first defense against revenue cycle friction.
Once a patient's information is registered, the next critical step is proactive insurance verification and securing pre-authorizations. This involves contacting the patient's insurance provider to confirm eligibility, coverage for the specific services planned, and details regarding co-pays, deductibles, and co-insurance. For many procedures and high-cost services, a pre-authorization is mandatory. Failing to secure one is a guaranteed denial. Integrating this verification step directly into the pre-appointment workflow is a non-negotiable part of modern medical charge capture. It prevents downstream denials and provides financial clarity for both the patient and the provider before services are even rendered.
This pillar represents the moment of truth for charge capture: the clinical encounter itself. The accuracy of billing is entirely dependent on the quality and specificity of the physician's and clinical staff's documentation. Every diagnosis, procedure, treatment, and supply used must be documented clearly and precisely in the patient's medical record.
This documentation serves as the legal record of the encounter and the ultimate source for all billing codes. Vague or incomplete notes create ambiguity for medical coders, leading to under-coding (and lost revenue) or over-coding (and compliance risks). Educating clinical staff on the financial implications of their documentation is a key strategy for improving the entire charge capture medical billing system.
The core charge capture process is where documented services are formally translated into billable charges. This can happen in several ways. In traditional, manual systems, physicians might fill out a paper superbill or encounter form, checking off the services they provided. In modern practices, this process is increasingly automated through the Electronic Health Record (EHR).
As a clinician documents a visit in the EHR, the system can automatically suggest the appropriate CPT® (Current Procedural Terminology) and ICD-10 (International Classification of Diseases) codes. These charges are then compiled from a facility's Charge Description Master (CDM), a comprehensive list of all billable items and their associated prices. A well-maintained CDM and an optimized EHR workflow are critical for ensuring every service is captured efficiently and accurately.
With the services documented and charges initiated, the next pillar involves the specialized task of medical coding and charge entry in medical billing. Professional medical coders review the clinical documentation to verify, correct, or assign the final billing codes. They ensure that the selected CPT, HCPCS Level II, and ICD-10-CM codes accurately reflect the services provided and are supported by the physician's notes.
Once codes are finalized, they are formally entered into the practice management system. This charge entry step creates the line items that will appear on the final insurance claim. Precision here is paramount, as incorrect codes are a primary reason for claim rejections and audits.
A claim is essentially an invoice sent to an insurance company. After charge entry, the compiled charges are formatted into a standardized claim file (like the CMS-1500 or UB-04). However, before this claim is sent to the payer, it must undergo a crucial "scrubbing" process.
Claim scrubbing uses specialized software to check the claim for common errors. This includes looking for invalid diagnosis codes, mismatched procedures and diagnoses, missing patient information, and formatting issues. This automated review catches countless potential errors that would otherwise lead to instant denials. This proactive quality check is a vital part of an efficient charge capture revenue cycle, saving significant time and resources on the back end.
Effective charge capture doesn't end when a claim is sent. The pillar of reconciliation and auditing is about closing the loop to ensure integrity and find leaks. Charge reconciliation is the process of comparing captured charges against multiple sources—such as appointment schedules, clinical documentation, and submitted claims—to ensure that every billable event was indeed captured and billed.
Regular audits, both internal and external, should be a standard part of your operations. These audits systematically review the charge capture process from beginning to end, identifying patterns of missed charges (revenue leakage), incorrect coding, or workflow inefficiencies. This is where you calculate and track your billing capture rate to measure performance. For a deep dive into data quality, trustworthy resources like [external link to a relevant AHIMA article on data quality] provide excellent standards.
Technology is the force multiplier that supports and enhances every other pillar. Modern EHR and Practice Management (PM) systems are at the center of the medical charge capture ecosystem. They provide the platforms for documentation, automated code suggestions, claim scrubbing, and reporting.
Specialized charge capture software can further automate the process, using rules-based engines to ensure compliance and accuracy. Furthermore, understanding the specific functionalities of your system is key. For example, knowing what is charge capture in Epic involves utilizing its specific workqueues and reconciliation tools to manage charges effectively. Leveraging technology to its fullest potential reduces manual errors, increases efficiency, and provides invaluable data for process improvement.
Even the best systems face challenges. The final pillar is about proactively identifying and overcoming these common hurdles to maintain a flawless charge capture medical billing workflow.
Charge leakage is the silent killer of profitability. It occurs when billable services are performed but never captured. This can be due to poor documentation, manual entry errors, or a failure to bill for supplies and injections. Implementing strong reconciliation processes is the primary defense.
This includes both undercharging (missing complexity, costing you money) and overcharging (a serious compliance risk). Both often stem from poor documentation or a lack of coder expertise. Regular training and audits are essential to ensure accuracy.
The longer it takes to capture and submit a charge, the longer it takes to get paid, negatively impacting your Days in A/R. Setting clear goals for "charge lag" (the time from service to charge entry) and monitoring this KPI can help streamline your operations.
When clinicians and billers operate in silos, misunderstandings and errors are inevitable. Creating a collaborative environment where coders can query physicians for clarification and physicians understand the billing implications of their work is crucial for success.
Achieving excellence in charge capture requires a commitment to continuous improvement. Implementing these best practices can significantly enhance your workflow and financial outcomes.
The ultimate goal of optimizing the charge capture revenue cycle is to improve financial performance. Success can be measured through several key performance indicators (KPIs) that provide a clear picture of your system's health.
The billing capture rate is a primary KPI that measures the percentage of billable services that are successfully captured and submitted on a claim. It's calculated by comparing the total value of captured charges against the potential value of all services rendered. A low capture rate is a direct indicator of revenue leakage and signals a need for immediate process improvements.
While some claim denials are inevitable, a high denial rate, particularly for reasons related to front-end errors like registration or authorization, points to significant weaknesses in the initial pillars of your charge capture process. Analyzing the root cause of denials provides a roadmap for targeted improvements.
This KPI measures the average number of days it takes to collect payment after a service is performed. An efficient charge capture process—with minimal charge lag and clean claims—directly leads to a lower Days in A/R, meaning cash flows into your practice faster. To learn more about the intricacies of coding that affect this, consider reading our [internal link to our blog on understanding medical coding].
The evolution of charge capture is heading towards greater intelligence and automation. Artificial Intelligence (AI) and machine learning are no longer concepts of the future; they are being implemented today. Imagine AI tools that scan clinical documentation in real-time and predict missing charges based on the notes. These systems can flag potential under-coding or suggest additional billable items that a human might have missed, ensuring maximum reimbursement while maintaining compliance. Predictive analytics can identify high-risk claims for denial before they are even submitted, allowing your team to intervene proactively.
Technology and processes are only part of the solution. The most successful healthcare organizations build a "charge capture culture" where every single employee understands their impact on the revenue cycle. This means moving beyond simply telling physicians to "document better." It's about showing them the direct financial impact of their work through clear, concise reports. It's about celebrating teams that achieve low denial rates and fostering an environment of shared responsibility for the organization's financial health. When everyone, from the front desk to the clinical floor to the back office, sees themselves as a guardian of the revenue cycle, the entire system becomes stronger.
A charge capture is the fundamental process of recording and documenting all billable services provided to a patient. It translates clinical activities (like consultations, procedures, and tests) into financial charges that are then used for billing the patient and their insurance provider.
In Epic, one of the most widely used EHR systems, charge capture is managed through a combination of automated and manual tools. Charges can be triggered automatically based on clinical documentation in Hyperspace, entered manually by clinicians via "charge routers," or managed by billers in specialized "workqueues" designed to review, correct, and process charges before they go to the billing system.
The billing capture rate is a key performance indicator (KPI) that measures the effectiveness of your charge capture process. It calculates the percentage of revenue from all billable services that is successfully captured and included in claims for reimbursement. A rate below 98-99% often indicates significant revenue leakage.
Charge entry is the specific administrative step where finalized medical codes (like CPT and ICD-10) and their associated fees are formally entered into the practice management or billing software. This action creates the detailed line items that form the basis of the insurance claim.
Ultimately, charge capture medical billing is far more than an administrative chore. It is the engine of your revenue cycle. By building a robust system founded on the nine essential pillars—from meticulous registration to insightful auditing—you transform this process from a potential liability into a strategic superpower. A flawless charge capture workflow not only maximizes revenue and accelerates cash flow but also strengthens compliance, reduces administrative waste, and builds a sustainable financial foundation for your practice's future.

In the complex ecosystem of healthcare, the financial health of your practice is just as critical as the well-being of your patients. The medical...
The medical billing process is a foundational system within any healthcare practice, responsible for converting patient services into financial...

In the complex world of healthcare, the terms "patient experience" and "patient satisfaction" are often used as if they mean the same thing. However,...