Text-to-Pay in Veradigm with Curogram
💡 Text-to-pay in Veradigm helps imaging centers collect payments faster and reduce admin work. This mobile payment method sends secure links...
14 min read
Jo Galvez
:
Updated on January 17, 2026
Table of Contents
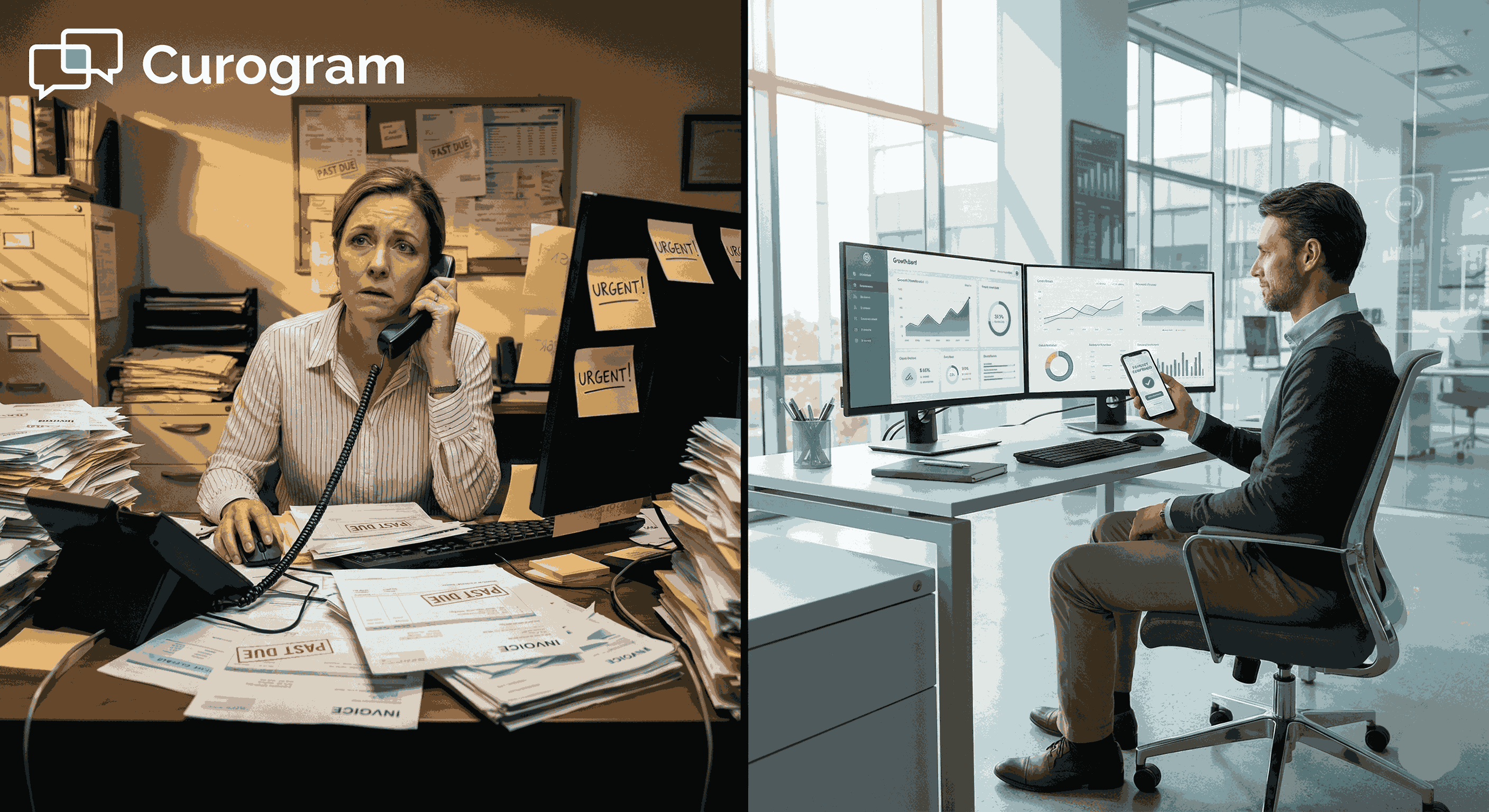
Billing delays cost imaging centers thousands of dollars each month. Staff spend hours calling patients about unpaid bills. Patients ignore paper statements because they arrive weeks after the visit. This cycle drains time, money, and staff energy.
Most imaging centers still use old billing methods. Front desk teams make dozens of calls each day. Billing staff mail hundreds of paper statements. These tasks take staff away from patient care and other key work.
Text-to-pay offers a better way. It helps centers collect payments from Veradigm systems without adding work for staff. The system sends secure payment links through text messages. Patients can pay right from their phones in just seconds.
This shift makes a real difference. Centers see faster payments and fewer unpaid bills. Staff stop spending hours on phone calls. Patients get clear, simple payment options they can use anytime.
Payment workflow automation works best when it fits into daily routines. For imaging centers using Veradigm, text-to-pay connects right to existing systems. There are no complex setups or new tools to learn.
The results speak clearly. Centers reduce aging balances by 30% or more. Cash flow becomes more stable week to week. Patient satisfaction goes up because billing feels easier and clearer.
For multi-site imaging networks, the benefits multiply. Every location follows the same billing process. Teams spend less time on manual follow-up. Financial teams get better visibility into collections across all sites.
This guide shows how text-to-pay solves real billing problems. You'll see how it speeds up collections, cuts staff workload, and improves patient experience. Whether you run one center or a large network, these workflows can help your team work smarter.
Imaging centers face unique billing challenges every single day. Each center handles hundreds of patients weekly. Many visits involve complex insurance claims. Staff juggle multiple payment sources, pre-approvals, and patient balances all at once.
Traditional billing creates serious bottlenecks. Front desk teams manually enter payment data. Billing staff print and mail thousands of statements monthly. Phone lines stay busy with patients asking about their bills. This work never stops, yet it rarely gets faster or easier.
Manual processes lead to predictable problems. Bills arrive late because printing and mailing takes time. Patients forget about balances when weeks pass between service and statement. Collections slow down as bills age without action.
Staff burnout becomes a real concern. Teams spend 40% of their day on billing tasks instead of patient care. Phone calls interrupt other work constantly. The same conversations happen over and over: explaining bills, taking card numbers, sending new statements.
Paper billing costs add up quickly. Each mailed statement costs around $1.50 when you include printing, envelopes, and postage. For a center sending 2,000 statements monthly, that's $36,000 annually. These costs keep rising as postal rates increase.
Patients expect modern payment options. They pay other bills online or through apps. They book appointments through websites. But when it comes to medical bills, they often face outdated processes that feel clunky and slow.
This gap affects patient satisfaction scores. Surveys show 68% of patients want digital payment options. They prefer text or email over phone calls. They want to pay immediately, not wait for statements to arrive by mail.
Multi-location networks face extra hurdles. Each site might follow different billing procedures. One location calls patients, another mails statements, a third uses both. This creates confusion and makes it hard to track performance across sites.
Financial planning becomes difficult without clear data. When collection times vary wildly, cash flow predictions fail. Revenue teams cannot forecast accurately. This uncertainty makes it harder to plan staffing, equipment purchases, or expansion.
Compliance adds another layer of complexity. Staff must protect patient data during every billing interaction. Paper statements can get lost or seen by others. Phone calls risk exposing information if security steps are skipped.
These problems compound in high-volume settings. Busy imaging centers cannot afford delays. Every hour spent on manual billing is time not spent serving patients. Every delayed payment affects the bottom line and operational stability.
The need for change is clear. Centers must find ways to speed up collections. They need to reduce manual work without cutting staff. They have to meet patient expectations while maintaining security and compliance.
Text-to-pay addresses these exact challenges. It automates billing reminders so staff don't have to call. It delivers payment links instantly so patients can act right away. It works with Veradigm systems so teams don't need new platforms.
This approach gives imaging centers what they truly need: faster payments, less staff burden, and happier patients. The workflow changes are minimal. The benefits show up quickly. Centers can finally move past outdated billing processes that hold them back.
Automation transforms how imaging centers handle payments. Instead of relying on staff to remember follow-ups, the system works on its own. Text messages go out at the right time, every time, without fail.
This consistency matters more than most teams realize. When billing reminders arrive on schedule, patients respond faster. They don't forget about balances. They don't wonder if they already paid or if the bill got lost in the mail.
Manual outreach creates gaps. Staff get busy with other tasks. Patients slip through the cracks. Follow-up calls happen inconsistently or not at all. These gaps cost centers real money as balances age.
Automated text-to-pay systems fix this problem at its source. The system tracks when balances become due. It sends secure payment requests through text the moment patients can pay. No waiting, no delays, no missed follow-ups.
Timing affects payment rates dramatically. Studies show patients pay 3x faster when they receive requests within 24 hours of service. Text-to-pay makes this timeline easy to hit every single time.
This speed reduces aging balances significantly. Bills don't sit for 30 or 60 days before patients see them. Centers collect payments Veradigm users owe while the visit is still fresh in patients' minds.
Predictable cash flow follows naturally. When most patients pay within days instead of weeks, revenue becomes steady. Finance teams can plan better. Imaging networks know what to expect each week.
Making It Easy for Patients to Pay From Any Device
Payment friction kills collection rates. If patients have to log into portals, create accounts, or wait on hold, many simply give up. They mean to pay later, then forget entirely.
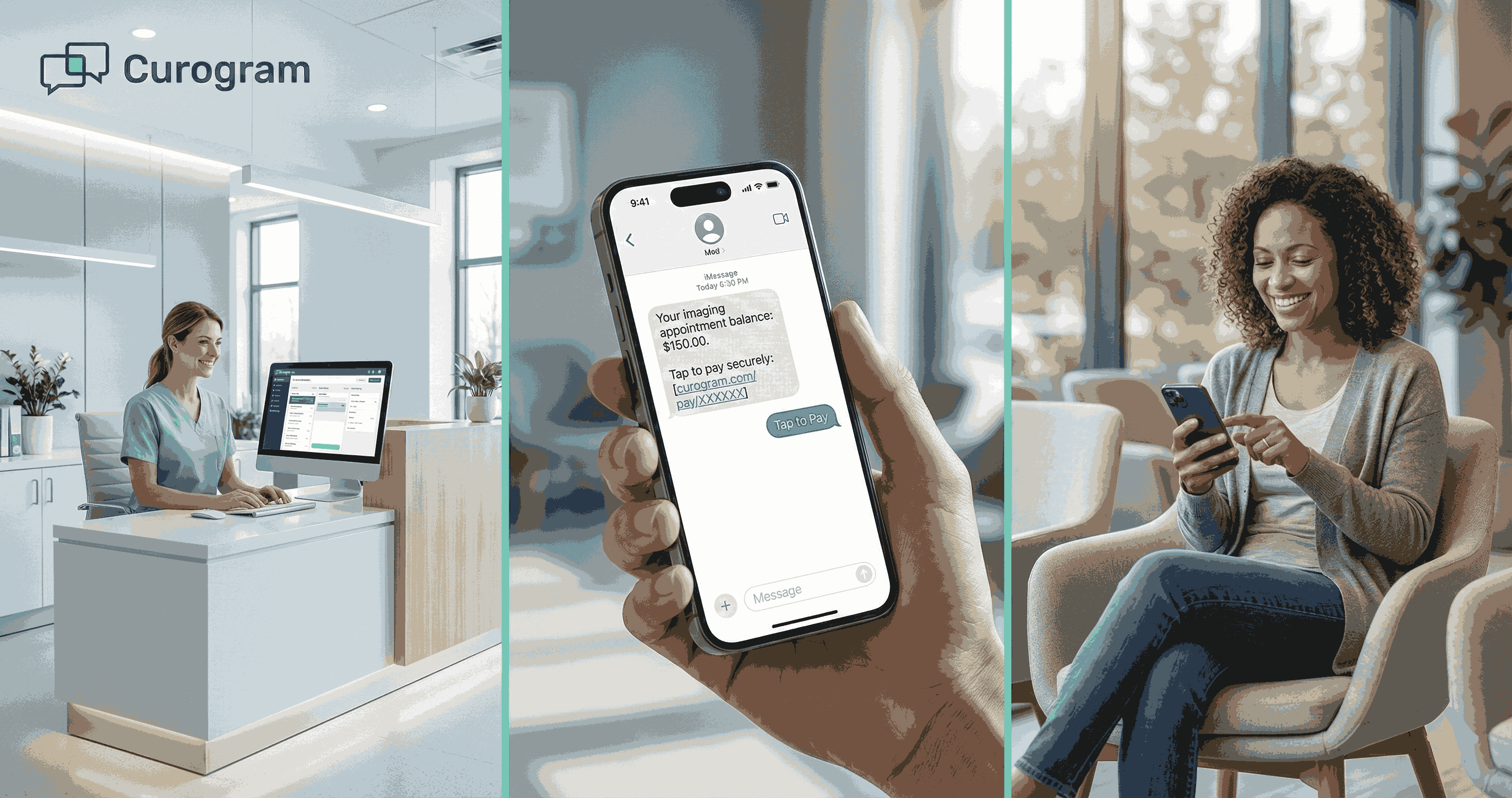
Mobile-friendly payment links remove these barriers. Patients tap the link in their text message. The payment page opens instantly on their phone. They enter their card info and confirm. The whole process takes under a minute.
This simplicity matters enormously. Over 85% of patients have their phone within reach all day. They check texts constantly. When a payment link arrives, they can act immediately without switching devices or finding login credentials.
The revenue cycle speeds up as a direct result. Payments that used to take 45 days now happen in 5. Staff stop chasing balances because most patients pay on their own. The system does the work automatically.
Multi-location imaging workflows improve across the board. Every site uses the same payment process. Patients at different centers get the same smooth experience. Management sees consistent collection rates network-wide.
Payment delays that once frustrated teams simply disappear. The combination of timely reminders and easy mobile access creates natural momentum. Patients want to pay. The system makes it effortless. Collections happen faster than ever before.
This workflow shift requires minimal training. Staff send payment links through existing Veradigm systems. Patients receive familiar text messages. The learning curve is nearly flat, yet the results are dramatic.

Administrative work drains imaging center resources daily. Billing teams make call after call. Front desk staff answer the same questions repeatedly. This cycle consumes hours that could support patient care or other vital tasks.
The numbers tell a stark story. Average billing staff spend 6-8 hours daily on collection calls. They reach only 30% of patients on the first try. They leave voicemails that often go unanswered. This inefficiency costs centers roughly $50,000 annually per full-time billing person.
Text-to-pay changes this equation completely. Automated billing reminders replace most collection calls. The system handles routine follow-ups without any human intervention. Staff time gets freed up for complex cases that truly need personal attention.
Traditional collection processes depend heavily on individual staff members. Someone must remember to call. Someone must track who was reached. Someone must note when to try again. This system breaks down constantly under real-world pressure.
Imaging centers using automated text reminders see immediate relief. The system sends the first reminders automatically when a balance is posted. It sends second reminders after a set number of days. It continues this cycle until patients pay or accounts need escalation.
This consistency cannot be matched by manual processes. Every patient gets the same attention. No one falls through the cracks because a staff member got busy or sick. The workflow runs 24/7 without breaks or mistakes.
Staff productivity jumps significantly. Teams that once spent full days calling patients now handle those same volumes in an hour. They focus on patients who need payment plans or have insurance questions. Their work becomes more valuable and less repetitive.
Administrative efficiency improves across entire imaging networks. Each site follows the same automated schedule. Management gains clear metrics on reminder effectiveness. Decisions about billing strategy get backed by solid data rather than guesswork.
The impact shows up quickly in key metrics. Collection rates rise by 25-40% in the first month. Staff overtime decreases as call volumes drop. Patient complaints about billing fall because the process feels less aggressive and more helpful.
For multi-location operations, standardization brings huge benefits. Corporate billing teams can implement one workflow across dozens of sites. Training becomes simpler. Performance comparisons get easier. The entire network operates more efficiently.
Paper statements represent a massive hidden cost. Each statement requires printing, folding, stuffing, and mailing. Supplies must be ordered and stored. Equipment needs maintenance. Staff spend hours preparing batches for the post office.
The direct costs add up fast. A medium-sized imaging center mailing 1,500 statements monthly spends around $27,000 yearly just on postage and materials. This doesn't include staff time, which can add another $15,000 to the total.
Text-to-pay eliminates most of this expense. Digital reminders cost pennies compared to paper statements. There's no printing, no postage, no supplies to manage. The savings flow straight to the bottom line.
Phone calls create their own burden. Staff must track call times, log results, and schedule callbacks. Patients often miss calls and play phone tag for days. This back-and-forth wastes time for everyone involved.
Automated texts cut phone volume by 50% or more in most centers. Patients get their information immediately. They can respond on their own schedule. Staff make calls only when truly needed, not as routine follow-up.
This shift streamlines financial workflows dramatically. Billing teams process more accounts with the same staff. Response times improve. Patients get faster answers. The whole system runs smoother from start to finish.
Environmental benefits matter too. Reducing paper waste aligns with healthcare sustainability goals. Centers can market this green approach to environmentally conscious patients. It's a win for operations and public perception.
Radiology workflow automation extends beyond just billing. When staff spend less time on collections, they can improve other processes. Scheduling gets smoother. Patient intake becomes faster. The entire operation benefits from freed-up capacity.
Staff morale improves noticeably. Team members prefer helping patients over making collection calls all day. They feel more productive when their time goes to meaningful work. Turnover often decreases as job satisfaction rises.
The technology investment pays for itself quickly. Most centers recover their implementation costs within 3-6 months through reduced paper expenses and improved collections. After that, the savings continue year after year.
Network-level benefits multiply these gains. A 10-location imaging network might save $250,000 annually on paper and postage alone. Add in staff time savings, and the total impact reaches well into six figures.
These operational improvements create lasting change. Once teams experience automated workflows, they rarely want to go back. The old way feels slow and wasteful. The new approach becomes the standard that everyone expects.
Traditional billing statements confuse patients regularly. Medical codes, insurance adjustments, and multiple line items create visual clutter. Patients cannot quickly find their actual balance. They worry they might pay the wrong amount.
Text-to-pay messages cut through this confusion. The message states the exact amount due. It explains what the charge covers in plain language. Patients see exactly what they need to do next.
This clarity speeds up payment decisions. When patients understand their bill, they act quickly. When they feel confused, they procrastinate or call with questions. Clear communication removes the barrier to payment.
Imaging centers see fewer billing-related calls after implementing text-to-pay. Patient questions drop dramatically. Staff spend less time explaining statements. Patients feel more confident about their financial obligations.
Modern patients expect digital options for everything. They order food, buy clothes, and manage bank accounts through their phones. Medical billing should work the same way.
Patient communication automation aligns with these expectations. Text messages feel familiar and convenient. Mobile payment links work like other apps patients use daily. The experience matches what patients already know.
This modern approach improves satisfaction scores. Patients rate their billing experience higher when they can pay by text. They appreciate not having to call during business hours or wait for statements in the mail.
Long-term loyalty grows from these positive experiences. Patients remember when billing feels easy and respectful. They're more likely to return for future imaging needs. They recommend the center to friends and family.
Veradigm imaging centers benefit from stronger patient retention rates. When the entire experience—from scheduling to payment—works smoothly, patients have no reason to go elsewhere. Convenience becomes a competitive advantage.
Different locations often develop their own billing habits. One site might be aggressive with calls. Another might be passive with mailed statements. This variability makes network-wide performance hard to measure or improve.
Text-to-pay creates uniform processes instantly. Every location sends the same types of messages. Every patient gets the same payment experience. Managers can finally compare site performance fairly.
Operational predictability improves dramatically. Leadership knows what to expect from each site. Budgeting becomes more accurate. Strategic planning gets easier when financial performance is consistent.
Multi-location imaging workflows operate more efficiently. Staff training happens once, then applies everywhere. Best practices spread quickly across the network. The whole organization moves forward together.
Payment confusion slows down more than just collections. Scheduling teams hesitate to book patients with outstanding balances. Check-in takes longer when staff must discuss bills. Follow-up care gets delayed over payment concerns.
Clear, automated payment workflows prevent these bottlenecks. Staff know patients will receive payment reminders automatically. They can focus on clinical scheduling rather than financial status. Operations flow smoothly without constant payment discussions.
Radiology appointment communication stays steady and predictable. Patients book scans without billing friction. They show up on time because financial clarity exists. The schedule stays full without payment-related gaps.
Imaging teams maintain smoother daily operations overall. Less time spent on billing means more time for patient care. Equipment stays busy. Revenue per scan hour increases. The business runs at peak efficiency.

Radiology groups handle highly sensitive information daily. Patient health data and financial details must stay protected. Any breach creates legal liability, damages reputation, and erodes patient trust.
Text-to-pay systems must meet strict security standards. Messages need full encryption. Payment processing must comply with HIPAA and SOC 2 rules. Audit trails should track every transaction for compliance reviews.
These protections matter especially for enterprise operations. IT oversight requires complete visibility into payment workflows. Security teams need detailed logs. Compliance officers must verify that every step meets regulatory standards.
Veradigm users maintain strong security while improving efficiency. The right text-to-pay platform keeps data safe without slowing down operations. Staff work confidently knowing every transaction is protected and tracked.
Manual billing invites mistakes. Staff mistype amounts. Data gets entered in wrong fields. Charges get duplicated or forgotten. These errors frustrate patients and create extra work correcting them.
Automated payment workflows minimize these risks. The system pulls exact amounts from billing records. It formats messages correctly every time. Payment links connect to the right accounts without manual data entry.
This accuracy reduces administrative costs significantly. Less time goes to fixing mistakes. Fewer patients call to dispute incorrect charges. Financial records stay clean and reliable.
Imaging centers maintain accurate financial histories. Audits go smoothly. Reporting becomes easier. Management trusts the numbers because the system eliminates most human error.
Choosing the right text-to-pay platform matters. The system must integrate smoothly, scale easily, and maintain security without compromise. Curogram delivers on all three requirements while making implementation simple.
Curogram integrates smoothly with existing Veradigm communication patterns. Staff don't need to learn complex new tools. The interface feels familiar because it works within systems teams already use daily.
This seamless fit accelerates adoption dramatically. Training takes hours instead of weeks. Staff start using the system immediately. Resistance disappears when the technology feels like a natural extension of current workflows.
Operational friction drops to nearly zero. IT teams don't struggle with difficult integrations. Clinical staff don't juggle multiple platforms. Everything works together as one unified system.
Imaging centers experience immediate workflow improvement. Payment collections speed up within the first week. Staff workload decreases noticeably. The benefits start flowing before the learning curve even becomes a factor.
Large imaging networks need systems that scale. Curogram supports thousands of patient interactions daily without slowing down. The platform handles peak volumes easily, maintaining speed and reliability.
Text-to-pay scales without increasing staff workload. Whether sending 100 or 10,000 messages, the system works the same way. Growth doesn't require more billing team members.
Radiology workflow automation becomes more efficient across all imaging modalities. MRI centers, CT facilities, and ultrasound clinics all use the same payment system. This consistency simplifies management and reporting.
Enterprise imaging teams gain consistent financial performance. Every site hits similar collection rates. Network-wide metrics improve steadily. Leadership can set realistic goals knowing the system delivers predictable results.
Every payment request Curogram sends is encrypted and logged. This creates complete audit trails that satisfy compliance requirements. IT teams can review any transaction at any time.
The system protects against PHI exposure and billing discrepancies. Patient data never appears in unsecured channels. Financial information stays encrypted from start to finish. Risk drops while efficiency climbs.
Enterprise IT teams maintain full oversight. They can monitor system performance, track usage patterns, and verify security protocols. Control stays where it belongs while operations get easier.
Imaging centers reduce risk while improving cash flow. This combination—better security and faster collections—creates a real competitive advantage. Centers operate more safely and more profitably at the same time.
Text-to-pay solves real problems that imaging centers face every day. It speeds up collections without adding staff burden. Patients get modern, easy payment options they actually want to use.
The workflow changes are minimal, but the results are significant. Centers that adopt text-to-pay see faster cash flow within weeks. Aging balances drop by 30% or more. Staff spend less time on collection calls and more time on valuable work.
For multi-location networks, the benefits multiply. Every site follows the same process. Performance becomes predictable. Financial planning gets easier because collections become consistent.
Patient satisfaction improves when billing feels modern and respectful. People appreciate clear messages and simple payment links. They remember when healthcare providers make their lives easier rather than harder.
Security and compliance stay strong throughout. Every message is encrypted. Every transaction is logged. Centers meet regulatory standards while delivering better patient experiences.
Curogram enhances Veradigm with a secure, scalable payment system built specifically for enterprise radiology. The integration works smoothly. The technology scales easily. The results show up quickly in both collections and staff satisfaction.
This approach represents the future of medical billing. Automated, mobile-first, and patient-friendly. Centers that adopt it now gain advantages their competitors will struggle to match later.
The path forward is clear. Imaging centers need faster payments, lighter staff workload, and happier patients. Text-to-pay delivers all three without complex implementation or steep learning curves.
Your center can start benefiting immediately. The technology is ready. The process is simple. The results are proven across hundreds of imaging facilities.
Book a Demo to See Curogram + Veradigm in Action.
Text-to-pay connects directly to Veradigm billing data through secure APIs. The system pulls balance information automatically and sends payment links without manual entry. Staff work within their existing interface with no new platforms to learn.
Patients check phones constantly but may not open mail for days. Text messages arrive instantly with payment links patients can use right away. This convenience results in payment rates 3x higher than traditional billing.
Most centers reduce billing calls by 50-70% after implementing automated reminders. This saves 3-5 hours of staff time daily for medium-sized facilities. Teams redirect this time to complex cases and high-value tasks.
All messages use end-to-end encryption and never contain protected health information. Payment links direct to HIPAA-compliant secure pages. Every transaction creates audit logs for compliance reviews and meets SOC 2 standards.
The system sends scheduled follow-up messages based on your rules. After the automated sequence completes, accounts flag for staff review. This ensures patients needing personal outreach get it while automation handles standard cases.
💡 Text-to-pay in Veradigm helps imaging centers collect payments faster and reduce admin work. This mobile payment method sends secure links...
💡 Text-to-pay helps imaging centers improve cash flow with Veradigm by speeding up payment collection. It cuts down the time patients take to pay...

💡 Patient payment workflows help Meditab IMS teams collect payments faster and reduce staff workload. These workflows automate billing tasks that...