Is Texting HIPAA Compliant? Everything You Need to Know
In today's hyper-connected world, text messaging has become a dominant form of communication – quick, convenient, and almost universally adopted....
9 min read
Alvin Amoroso : Updated on April 30, 2025
.png)
HIPAA compliance forms the bedrock of patient trust in the healthcare system, establishing essential rules for safeguarding sensitive health information. Yet, rules on paper only gain power through active oversight and accountability. Who exactly wields the authority to ensure these critical standards are met? The answer isn't confined to a single office; understanding who enforces HIPAA requires exploring a network of federal agencies, state authorities, and internal organizational structures. Getting clarity on who is responsible for HIPAA enforcement is the crucial first step for any entity handling health data and for individuals seeking to understand their privacy rights. Understanding the answer to "who enforces HIPAA?" is fundamental for compliance.
Many assume a single entity holds this responsibility, but the reality is more nuanced. While one agency takes the lead for the critical Privacy and Security Rules, HIPAA enforcement involves a coordinated effort among multiple federal and state bodies, as well as responsibilities within healthcare organizations themselves. Fully grasping who is responsible for HIPAA enforcement is crucial not only for covered entities (CEs) and their business associates (BAs) striving for compliance but also for individuals seeking to understand their rights.
This comprehensive guide dives deep into the question, "Who enforces HIPAA?". We'll explore the primary federal authority, the expanding roles of other key players like State Attorneys General and the Department of Justice, unpack the intricate enforcement process, detail the potentially severe consequences of non-compliance, clarify internal responsibilities regarding who is responsible for implementing and monitoring the HIPAA rules, and answer frequently asked questions about who is responsible for enforcing HIPAA.
When asking what agency enforces HIPAA, particularly its core privacy and security components, the primary answer lies within the U.S. Department of Health and Human Services (HHS). While HIPAA originally focused heavily on health insurance reform (Title I, largely enforced by the Department of Labor and Treasury Department), its Administrative Simplification provisions (Title II) set the stage for crucial privacy and security standards. It's important to know that HHS oversees HIPAA compliance related to these Administrative Simplification provisions.
Within HHS, the Office for Civil Rights (OCR) is the key agency delegated with the authority to enforce the HIPAA Privacy Rule, Security Rule, and Breach Notification Rule. These rules govern how CEs (like health plans, healthcare clearinghouses, and most healthcare providers) and their BAs must protect PHI. For many practical purposes, OCR is the answer when asking what agency enforces HIPAA's privacy aspects. This agency oversees HIPAA implementation across the nation.
.png?width=600&height=400&name=who%20enforces%20hipaa%20%20(2).png)
OCR employs several methods to ensure adherence to HIPAA regulations:
While OCR handles the Privacy, Security, and Breach Notification Rules, another HHS agency, the Centers for Medicare & Medicaid Services (CMS), enforces HIPAA's Administrative Simplification Rules related to standardized electronic transactions, code sets, and unique identifiers (like the National Provider Identifier - NPI). Complaints regarding these specific transaction standards are often handled through CMS's Administrative Simplification Enforcement Testing Tool (ASETT). So, while OCR is a major player, CMS also contributes to the picture of who is responsible for enforcing HIPAA.
While OCR is the primary enforcer for privacy and security, they are not the only government body who is responsible for HIPAA enforcement. Two other key players significantly impact the enforcement landscape:
.png?width=600&height=400&name=who%20enforces%20hipaa%20%20(3).png)
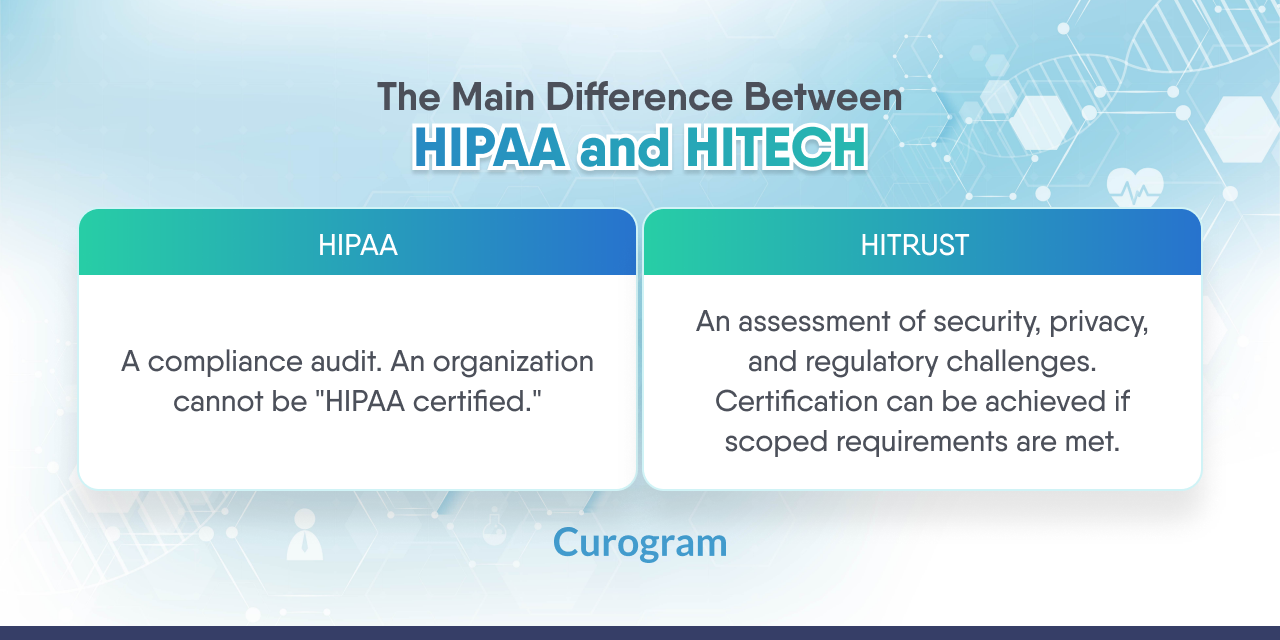
The Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 significantly expanded HIPAA enforcement by granting State Attorneys General the authority to bring civil actions in federal district court on behalf of state residents whose HIPAA rights have been violated.
While OCR and State AGs typically handle civil and administrative enforcement, the U.S. Department of Justice (DOJ) steps in for Criminal HIPAA violations. Section 1177 of the Social Security Act (42 U.S.C. § 1320d-6) makes it a federal crime to knowingly obtain or disclose individually identifiable health information (IIHI) in violation of HIPAA.
The involvement of State AGs and the DOJ demonstrates that the scope of who is responsible for HIPAA enforcement extends beyond administrative penalties, encompassing significant civil litigation and criminal prosecution power.
.png?width=600&height=400&name=who%20enforces%20hipaa%20%20(4).png)
Understanding who enforces HIPAA also involves knowing how enforcement actions proceed. The process generally follows these steps:
Failure to comply with HIPAA can lead to significant consequences imposed by the bodies who enforce HIPAA.
OCR imposes CMPs based on culpability:
(Note: The following dollar amounts are based on annual inflation adjustments estimated for early 2025. Always refer to the official HHS website or Federal Register for the precise current figures.)

Annual Penalty Cap: Approx. $2,250,000 for identical violations per year.
Factors Influencing Penalties: Harm, number affected, history, size, cooperation. Knowing these factors helps understand how the entities who enforce HIPAA decide on penalties.
While external agencies handle formal enforcement, the day-to-day responsibility for upholding HIPAA standards lies within each covered entity and business associate. A vital question arises internally: Who is responsible for implementing and monitoring the HIPAA rules? Clarity on who is responsible for implementing and monitoring the HIPAA requirements is essential for effective compliance programs.

Mandated by the Privacy Rule (§164.530), the Privacy Officer is responsible for implementing and monitoring the HIPAA privacy policies. Key duties include developing policies, training, handling patient rights requests and complaints, and acting as the OCR contact for privacy matters.
Mandated by the Security Rule (§164.308), the Security Officer is primarily who is responsible for implementing and monitoring the HIPAA Security Rule safeguards for ePHI. Key duties include developing security policies, conducting risk analyses, managing incidents, overseeing technical controls, and ensuring appropriate BAAs are in place. Understanding that the Security Officer is who is responsible for enforcing the HIPAA Security Rule internally is crucial for protecting ePHI. This role is central to the internal aspect of who is responsible for enforcing the HIPAA Security Rule.
One person may hold both roles in smaller organizations, requiring broad knowledge. Larger entities often separate these roles. Regardless of size, clear designation and resources are vital. Defining who is responsible for implementing and monitoring the HIPAA rules within the organization's structure prevents gaps.
Ultimately, HIPAA compliance is everyone's job. All workforce members must follow policies, complete training, and report issues. They play a part in the collective answer to who is responsible for implementing and monitoring the HIPAA standards daily.
Multiple federal and state entities enforce HIPAA. The primary enforcer for the Privacy, Security, and Breach Notification Rules is the Office for Civil Rights (OCR) within the U.S. Department of Health and Human Services (HHS). State Attorneys General also have authority to enforce HIPAA through civil actions. The Department of Justice (DOJ) handles criminal HIPAA violations. Additionally, the Centers for Medicare & Medicaid Services (CMS) enforces specific HIPAA rules related to transactions and code sets. Understanding what agency enforces HIPAA involves recognizing these different players.
HIPAA compliance is mandatory for two main groups: Covered Entities (which include health plans, healthcare clearinghouses, and healthcare providers who conduct certain electronic transactions) and their Business Associates (individuals or organizations that perform functions or activities on behalf of, or provide services to, a Covered Entity involving the use or disclosure of Protected Health Information - PHI). Subcontractors of Business Associates who handle PHI must also comply. Ultimately, both organizations and their workforce members are responsible for ensuring compliance with HIPAA rules applicable to their roles.
The HIPAA Security Rule is a national standard specifically for the protection of electronic Protected Health Information (ePHI). It requires Covered Entities and Business Associates to implement reasonable and appropriate administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of ePHI they create, receive, maintain, or transmit. This includes measures like access controls, encryption, risk analysis, and workforce training. Knowing the rule helps understand the duties of the person who is responsible for enforcing the HIPAA Security Rule internally.
These scenarios illustrate how the different bodies who enforce HIPAA act:
So, who enforces HIPAA? The answer is definitively multi-faceted. The HHS Office for Civil Rights (OCR) stands as the cornerstone, the primary entity who oversees HIPAA Privacy, Security, and Breach Notification Rules. However, the full picture of who is responsible for HIPAA enforcement must include State Attorneys General wielding civil authority and the Department of Justice tackling criminal acts. The question "who enforces HIPAA?" requires acknowledging all these players.
Furthermore, effective compliance hinges on internal diligence. Understanding who is responsible for implementing and monitoring the HIPAA regulations within an organization—typically designated Privacy and Security Officers supported by a trained workforce—is just as critical. Grasping this complex web of external agencies and internal duties, which collectively answer "who is responsible for enforcing HIPAA", is essential for navigating compliance, protecting data, maintaining trust, and avoiding severe penalties. Proactive management and a strong compliance culture are the best defense when considering what agency enforces HIPAA and how to meet their expectations.

In today's hyper-connected world, text messaging has become a dominant form of communication – quick, convenient, and almost universally adopted....
In medical practice, HIPAA compliance is non-negotiable. With the rapid adoption of conversational AI, new dimensions are added to the challenge....
The Health Insurance Portability and Accountability Act was enacted in 1996 to ensure the security of patient health records and other vital...