The #1 Cause of Administrative Burnout in Medical Practices
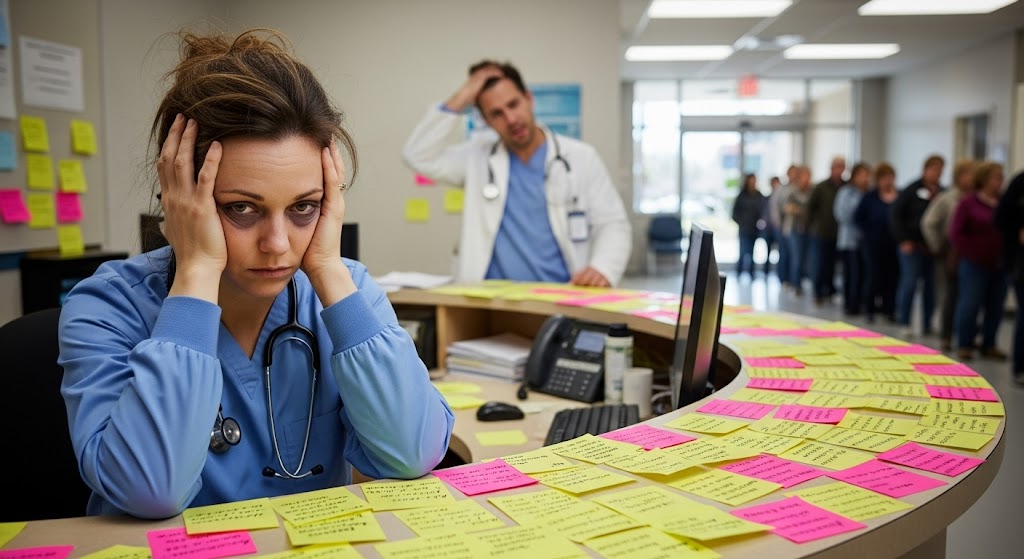
💡What causes administrative burnout in healthcare? Disconnected systems that force staff into manual work and endless phone calls are seen as the...
7 min read
Gregory Vic Dela Cruz : August 9, 2025

Medical practitioners often admit that patient care is a team sport. Like any high‑performing team, private practices win when the playbook is clear. Without standardized workflows, small operational hiccups create clinical risk: handoff details get lost, refill requests pile up, and lab results sit in inboxes unseen. Patients feel the delay; providers feel the cognitive load; the whole practice feels the friction.
This guide explains how clinical workflow optimization for private practices turns everyday processes into reliable systems. We’ll map the three highest‑impact flows—patient handoffs, prescription refills, and lab result management—then show you how to standardize, automate, and measure each. Expect practical frameworks (SBAR handoffs, refill triage ladders, and results routing rules), concrete role definitions, and quick‑start checklists to reduce error risk while improving speed and consistency.
If your team is ready to replace ad‑hoc “workarounds” with predictable care pathways, you’re in the right place. We’ll highlight the small changes that deliver outsized gains and point to tools that fit naturally into your existing EMR and team routines.
Want a guided walk‑through tailored to your specialty and staffing model? Read on to see how secure messaging, digital forms, and automated routing make these workflows click.
Begin by listing the clinical processes that touch most visits and create the most risk if delayed: patient handoffs (room‑to‑room, provider‑to‑provider, and care‑to‑billing), prescription refills (acute vs. chronic), and lab/diagnostic result management (normal vs. abnormal vs. critical). For each process, capture current state steps, handoff points, and failure modes (e.g., “refill denied due to missing BP” or “abnormal result not acknowledged within 24 hours”).
Embed triggers and rules into your tools. Examples: closing a note pushes an SBAR handoff to the next role; a refill request with criteria met auto‑generates a pending prescription for provider sign‑off; an abnormal lab code automatically creates a task with SLA and escalation logic.
By codifying the work and letting software handle the hand‑offs, private practices gain both clinical safety and operational tempo—with less cognitive burden on clinicians.
Before jumping into solutions, it’s important to understand exactly where—and why—private practices lose efficiency and introduce risk. Every delay, missed communication, or incomplete task has a ripple effect that impacts both patient care and staff workload. Below, we’ll break down the most common problem areas in clinical workflows, explain their root causes, and set the stage for how optimization strategies can resolve them.
One of the biggest threats to care continuity is inconsistent patient handoffs. In many practices, how information is shared depends entirely on the person doing the handoff. A nurse might mention a recent medication change but omit allergy updates. A provider might verbally update a colleague but forget to document the rationale for changing a treatment plan. This variability means critical details can slip through the cracks, leading to duplicate work, unnecessary tests, or even adverse patient outcomes.
Without a standardized handoff protocol, such as SBAR (Situation, Background, Assessment, Recommendation), staff rely on personal habits and memory. The problem is amplified during shift changes, provider coverage, or high-volume clinic days when cognitive load is at its peak.
Prescription refill requests often get trapped in a no-man’s-land between the patient’s call and the provider’s inbox. They’re buried in email threads, mixed into the EMR task list, or sitting in a shared fax folder. The lack of clear triage criteria means all refills are treated the same—whether it’s a straightforward renewal for a long-term medication or a high-risk controlled substance requiring provider review.
This bottleneck results in delays that frustrate patients, trigger repeat calls, and consume staff time. In worst-case scenarios, it interrupts treatment adherence, potentially impacting the patient’s health and increasing the likelihood of an urgent visit.
Lab and diagnostic test results—especially abnormal ones—demand timely review and patient communication. But in many private practices, result management is reactive and scattered. A critical result may be routed to a provider’s inbox while they’re out of office. A normal result may languish unacknowledged for days, leaving patients wondering about their status. The lack of automated routing rules, clear SLAs (service-level agreements), and escalation protocols creates risk for both patient safety and legal compliance.
When results are missed or delayed, it erodes patient trust, forces clinicians into “damage control” conversations, and increases malpractice exposure.
Fragmented communication is another major culprit. Information might live in the EMR, on sticky notes, in personal email accounts, or in a chat app. Each tool serves a purpose, but without integration and agreed-upon workflows, staff must constantly switch contexts to piece together a complete patient picture.
This patchwork approach increases the chance of missed messages, duplicated effort, and overall inefficiency. It also makes onboarding new staff harder because there’s no single “source of truth” for how the clinic communicates and completes tasks.
Finally, many practices operate without a real feedback loop for process performance. Cycle times for handoffs, refill approvals, and result acknowledgments are rarely tracked. Without data, delays feel “normal” and systemic issues remain hidden. Staff may assume a process is efficient simply because “we’ve always done it this way.”
Lack of performance metrics means there’s no objective way to identify bottlenecks, coach underperforming workflows, or celebrate improvements. The result is stagnation—where small inefficiencies accumulate into major operational drag over time.
At the core, these pain points exist because most private practices evolve organically rather than by design. Roles shift as staffing changes; new tools are added without process redesign; protocols are informal and stored in people’s heads rather than the clinic’s systems. This “accidental workflow” environment depends on individuals rather than reliable structures, making it fragile and prone to error.
The good news: these problems are solvable with deliberate private practice optimization. Standardizing communication, embedding protocols into tools, and automating routine steps can remove variability and restore control. In the following sections, we’ll show how to apply these principles to three high-impact workflows—handoffs, prescription refills, and result management—so your team can deliver safer, faster, and more consistent patient care without adding to the workload.
If you'd like to learn more about improving healthcare workflow management for small clinics, we've previously covered that, including why it's key to the patient experience.

Choose SBAR (or IPASS) and make it universal—providers, nurses, MAs, and care coordinators. Create a one‑minute template with required fields and smart prompts. Example SBAR card: Situation (why handoff), Background (diagnoses, meds, allergies), Assessment (what changed, vital flags), Recommendation (next step + time expectation).
With this private practice optimization approach, handoffs stop being variable emails or verbal “drive‑bys” and become reliable, auditable transitions that protect patients and provider time.
Paired with your EMR, Curogram reduces back‑and‑forth phone calls, shortens cycle times, and creates a defensible record of communication—core wins for private practice optimization.
This is private practice optimization at its most tangible: fewer phone tags, faster patient answers, and clearer accountability. Patients feel informed; clinicians feel in control; risk is reduced.
Optimizing clinical workflows isn’t about adding work; it’s about removing variability. With standardized handoffs, protocolized refills, and disciplined result management, your private practice can deliver faster answers, fewer errors, and more confident care.
Tools matter too. Curogram’s HIPAA‑compliant messaging, digital forms, after‑hours auto‑responders, and read receipts help your team communicate clearly, capture the data you need, and prove the work you’ve done—all without extra clicks.
Want to see what these streamlined workflows look like? Request a Curogram demo today.
💡What causes administrative burnout in healthcare? Disconnected systems that force staff into manual work and endless phone calls are seen as the...

Compliance is never optional in the healthcare industry. For small medical practices, this means implementing HIPAA-compliant workflows that...

Running a small clinic is centered around quality care for each and every patient. But what looks easy from the outside, is in reality juggling a...